Stephen Kreitzman Ph.D, (UK Registered Nutritionist) & Valerie Beeson
Howard Foundation Research Ltd. Cambridge
Weight loss goals are not utopian dreams. Diabetics off their drugs in days. Blood pressure reduced.
Patients qualifying for elective surgery. Depression tempered. Fertility enhanced. Patients capable of a more active lifestyle.
Blood lipid profiles improved. Self esteem and quality of life enhanced. These are goals achieved routinely by weight loss.
They are being achieved by your GP colleagues and by your pharmacist colleagues. And it isn’t necessary to wait for PCT funding.
Obesity management is basic science. People have to eat a lot fewer calories than they use. That is, they have to maintain a large calorie gap. Calories do count and the laws of physics can not be violated regardless of the macronutrient profile of the foods eaten.
EXERCISE
Obesity management also requires more than exercise at the levels realistically achievable by seriously overweight people. Obesity management requires an understanding of the full impact of extra ener-gy expenditure – even in the unlikely event that the extra expenditure is substantial – when energy intake continues to be excessive. Obese people have eaten and in all probability are still eating more calories than they need.
Their excess intake can often be measured in the many hundreds of calories. It takes a very large amount of exercise to cope with these excess food calories before any contribution can be made from the body’s fat stores and cause weight loss. After coping with the excess food calories, it takes an additional deficit of 3500 calories to consume a single pound of body fat. Often it takes a major effort for obese people simply to accomplish activities that other people take for granted. To expect obese people to dissipate very large numbers of excessive calories by exercise is naïve. To risk the heat overload generated by intensive exercise in people whose fat mass, a considerable and effective insulation material, dangerously impedes heat loss, is unwise.
WEIGHT MANAGEMENT IS ACHIEVABLE
Weight loss of significant magnitude, even in seriously obese patients, is achievable either in your own practice or with the assistance of a rapidly growing number of trained pharmacists. Pharmacists over the last 3 years are getting excellent
results running the same professional Lipotrim prot-ocols as have been run exclusively in UK general practices and hospital clinics since 1987. The parliamentary all party pharmacy group (APPG) has called for greater pharmacy
involvement in obesity management and pharmacists are responding to that call.
PHYSIOLOGY
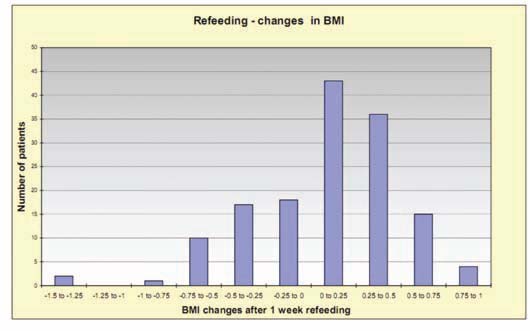
There are some fundamental concepts of physiology that must be understood in order to treat weight problems successfully. The most frequently misunderstood concept, even by professionals, is the rela-tionship between weight loss and body fat loss. They are not the same. Weight loss can be achieved with a diuretic, by sweating and even by exercise, without any loss of body fat. The primary fuel providing energy for the body is glucose and it’s reserve polysaccharide, glycogen. These carbohydrates are stored in the body in the liver, muscles and fat cells. Fat people can store a considerable amount of glycogen in their numerous fat cells, in comparison with thin people who usually only store about a pound or two of this carbohydrate fuel. It is extremely important to recognize that the carbohydrate fuel is stored in a highly hydrated state – 3-5 parts water to each part of glycogen. This results in what amounts to a diuresis as glycogen is utilized. Instead of 3500 calories required per pound of fat weight lost, weight lost as glycogen and its associated water requires only about 360 Calories per pound, 10% of the energy deficit. Further, repletion of glycogen and water weight is rapid and necessary. Shifting glycogen and water weight on and off should not be confused with obesity management.
WEIGHT LOSS USING NUTRITIONAL REPLACEMENT THERAPY
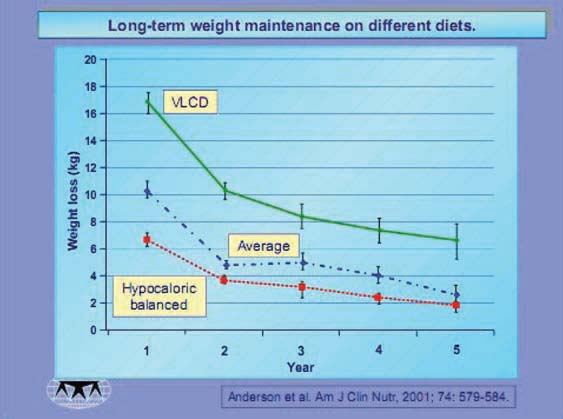
Obesity management requires enough of a calorie deficit to deal with 7700 kcal per kg of fat weight lost. An individual of
average height has to lose about 3 kg of weight to reduce BMI by a single unit. Therefore a calorie deficit of energy use
compared with intake has to reach about 23,100 kcal in order to achieve one unit reduction in BMI. This can most
realistically be achieved by maximizing the calorie gap between intake and expenditure. The absolute maximum is obviously achieved by a total fast, however, a total fast provides no essential nutrients and would therefore lead to serious health problems and ultimately death. Energy intake is not required since each stone of excess weight is a store of over 37,000 kcal. Providing the essential nutrients of vitamins, minerals, trace elements, essential amino acids and fatty acids entails providing some calories, therefore the maximum safe caloric gap is defined by the calorie content of an intake providing all essential nutrients in adequate amounts. This is achieved, by a carefully designed formulation, in approximately 400 kcal per day. Nutritional replacement therapy formulations have a long history of safe and effective maintenance of patients for prolonged periods, however, they are ordinarily designed to provide enough energy for weight maintenance or even weight gain. Drastic elimination of fat calories from these formulations, however, can provide for essential nutrition while supporting sustained weight loss. This is the basis for the success of the Lipotrim obesity management system.
OVERCOMING “ADDICTIVE” EATING BEHAVIOUR TO ACHIEVE LIFESTYLE CHANGE
It is becoming increasingly apparent that excessive consumption of food shares many of the characteristics of addictive behaviours towards other substances of abuse.
Whether it be tobacco, alcohol or drugs, once excessive consumption is evident, the only way to have any reasonable chance of regaining control is to stop completely the substance being abused. While total abstinence is achievable and
generally recommended when dealing with these other substances, obese patients are usually encouraged to control their excesses by consciously overriding their drives to eat in the face of the temptations of continued exposure to food. The frequent failure to achieve this over a prolonged period is not surprising. What is required is a complete withdrawal from the lure of food for as long as possible. This is achievable using a nutritional replace-ment formulation, which is not generally perceived as food. When food avoidance is complete, it has the dramatic effect of re-establishing more cont-rolled behaviour towards food when traditional food is reintroduced. This positive benefit is commonly seen, for example, when people substitute skimmed milk for whole milk in tea or coffee. It is rare for these people to reintroduce whole milk again. Long term lifestyle change in eating behaviour becomes considerably more likely when there is a complete break from the substance of abuse. Patients adhering strictly to the Lipotrim total food replacement formulations have a vastly improved record of post diet weight control compared with historic approaches.
ADVANTAGES OF PHARMACY OVER IN-HOUSE TREATMENT
While many prac-tices prefer to manage their own obese patients with Lipotrim, there are practical limitations that often
make it desirable to utilize a pharmacy. In addition to the obvious considerations of time availability, where a pharmacist could treat a patient at almost any time during long opening hours, time available in the surgery is generally much more constrained. As a result, treatment is often restricted to the most severe cases where the weight has contributed to some co-morbid condition such as diabetes or when the patient faces a long delay in attaining surgical help unless weight is lost. With almost a quarter of the adult population now clinically obese and over half of the population overweight, the treatment burden can rapidly become overwhelming for the practice. Also, it is widely recognized that prevention by intervention before the patient becomes obese is preferable. Weight is not considered a medical problem below BMI30 and it is hard to justify practice time for lower weight patients who are otherwise still heal-thy. Similarly, once a patient has achieved weight loss and is at a normal weight, they are greatly in need of further, long term maintenance assistance, but this is difficult to justify in practice since they are now at a normal weight. There are, however, some medical conditions where either total management in practice or a shared management with the pharmacist is necessary. This is most dramatic with type II diabetes treated with oral agents. There is a p r e c i p i t o u s normalization of blood sugar, usually within the first 3-5 days of Lipotrim treatment. Continued use of the oral agents in the presence of normal sugars can become problematic and therefore medication needs to be stopped or severely reduced. This cannot be done by the pharmacist without the cooperation of the primary care doctor.
THE FACTS ARE IN THE LITERATURE
Obesity has finally become recognized as a major public health problem and the primary care team is being looked upon
to deal with it. The approach to obesity treatment briefly outlined in this short piece is extremely well documented in what has become a vast scientific and medical literature. Weight losses of about 1 stone per month for women and even
more for men are not only achievable, but are also expected. They are proven safe when used under knowledgeable
care and there is no longer any excuse for patients to endure futile attempts to manage their obesity. Considerable
discussion of the medical science can be found on the UK Food Education Society web site at www.foodedsoc.org.
PDF version: 2-5-successful