Tag Archives: pharmacy-based programme
Treating obesity is easy – just eat less (so the saying goes)
Assuring there will be a ‘tomorrow’s pharmacist’
Vending machines for prescription drugs are already here. How much longer will you be here?If you intend to be a pharmacist of tomorrow, you need to start acting today. Delivering a professional weight management service is a good place to start
By Dr Stephen Kreitzman Ph.D, RNutr and Valerie Beeson, of Howard Foundation Research
THE ROYAL PHARMACEUTICAL SOCIETY has set out best practice standards for pharmacies delivering public health services in England and Wales. The ‘Professional standards for public health practice for pharmacy’ were created in partnership with the Department of Health, Royal Society for Public Health and Faculty of Public Health, and focus strongly on backing up services with data. They call on pharmacists to ensure their public health offering is evidence-based, tailoring it to local needs wherever possible, and to gather data that proves the value of services
Of all the important services being offered in pharmacy, it could be argued that weight management is the most valuable and documentable. It is valuable because controlling weight prevents and can even treat type 2 diabetes, high blood pressure, depression, sleep apnoea, poor fertility and a host of other health issues that are prevalent in the community. It can even impact on services such as smoking cessation, since the possibility of weight gain is often a reason for failure to stop smoking.
A weight management service is readily documentable, since tracker software is available that will instantly provide evidence for weight loss achievements and medical benefits from the weight loss. If you can’t produce data, you have no proof of your pharmacy’s accomplishments.
The not-yet-obese
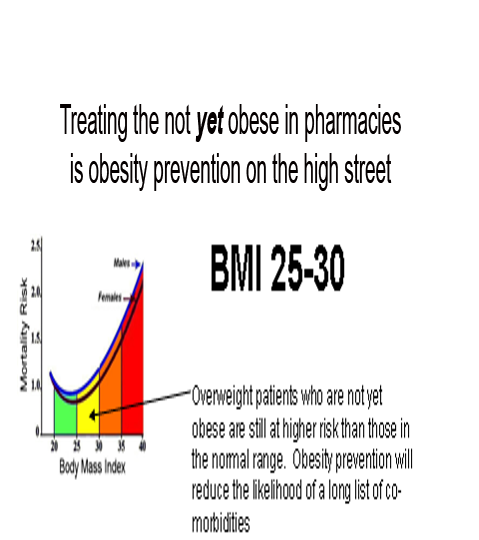
Treating overweight, but not-yet-obese, people in pharmacy, is obesity prevention on the high street. There are over 30 million overweight and obese people in the United Kingdom. Since no one ever became obese without first being overweight, it is important to provide real help to people at this stage. It is much less problematic to help people who do not have a massive amount of weight to lose and who also do not yet have some of the serious medical consequences associated with excess weight.
Pharmacy has become the prime location for weight management in the UK and Ireland. With the NHS ‘Call to Action’, pharmacy professional bodies are urging pharmacists to make their voices heard and shout about the good they do in improving people’s health.
Helping people lose weight is not just about making them feel good but is also about preventing major long-term health problems, such as type 2 diabetes. A recent article in GP magazine reported a staggering seven-fold rise in insulin use in type 2 diabetes over a nine-year period. An effective pharmacy weight management service could have an enormous and immediate benefit.
But it seems that it’s not just the NHS that needs to hear what pharmacy has to say. The public do, too. North London LPC was inundated with enquiries about a newsletter it had produced raising awareness of pharmacy services in the area.
Promote your service
So what does that mean to you as a pharmacist with a team already offering an established weight management service? Promote your service far and wide and show the public and the NHS what you’ve been doing to improve the health of the nation.
Fin McCaul, for example, is first and foremost a community pharmacist practising in Manchester. He is also the chairman of the Independent Pharmacy Federation and works for Bury CCG one day a week as its long-term conditions lead.
Fin’s passion for independent pharmacy is second only to helping patients lose weight and stop smoking. With an average of 100 quits per year and well over 1,000 patients helped through the weight loss service in his pharmacy, there is nobody better placed to talk about the opportunities and challenges for pharmacy now that public health commissioning has moved into the care of local authorities.
Delegation, motivation and marketing skills and advice for pharmacists and their team are just some of the benefits from his stop smoking/weight loss clinics. At the 2013 Pharmacy Show Mr McCaul organised a series of patient services workshops delivered by pharmacists who were successfully running weight services in their local community and wanted to share their knowledge and expertise. At the March 2014 Independent Pharmacy Federation conference, Fin again provided the opportunity for training in critical pharmacy services and the weight management clinic run by author Valerie Beeson was well attended and appreciated.
A giant change in practice
NHS England’s education arm has launched new standards for pharmacists delivering patient consultations, which have been hailed as a “giant change” in pharmacy practice. Health Education England (HEE) called on pharmacists to ensure they were educating patients, building a relationship with them and respecting their individual needs when conducting consultations.
The Westminster Food and Nutrition Forum seminar, held in London in February, kicked off with the staggering statistic that more than half of the UK population could be obese before 2050. This could create costs of £50 billion a year to the NHS, warned speakers, who included representatives from NHS England, Public Health England, NICE, the Department of Health, CCGs and the nutrition sector.
The speakers agreed that primary care is the key battleground for tackling the issue. But with GPs and pharmacists at the frontline of delivering public health services, who is better placed to keep the nation’s waistline under control? It is clearly pharmacy.
There was no doubt that pharmacy should offer obesity services. Ash Soni, pharmacist and vice chair of the RPS English Pharmacy Board argued that most overweight people did not feel unwell so would usually fail to see the point of visiting their GP. Mr Soni believed using a medical model was the wrong starting point. Most people visited pharmacies for multiple reasons, which presented an “ideal opportunity.”
Pharmacy is an excellent provider of weight services for the community. Many overweight people in the BMI 25-30 range take advantage of pharmacy weight loss programmes, recognising that they really work and feeling confident that they are being monitored by healthcare professionals. Pharmacists’ expertise in weight management, however, has proven extremely valuable for the treatment of obese and even morbidly obese people. This is a group who could have qualified for bariatric surgery at great expense and risk.
Effective weight loss absolutely needs to be monitored by knowledgeable healthcare professionals, because real weight loss is not benign. Type 2 diabetics, for example, who lose weight by compliance with a total food replacement diet programme, will induce remission of their diabetes within a few days and continuing with hypoglycaemic medication can result in hypoglycaemia.
There are multitudes of patients taking drugs with a very narrow safety spectrum, such as warfarin or lithium. Dieting can alter the absorption of these drugs, so dosages need to be carefully monitored. There are some people who really should not be dieting at all. Pregnant women, patients with a recent history of surgery, stroke or heart attack are not logical candidates for weight loss.
Weight maintenance requires attention and is not usually possible in a busy medical practice. Long-term support in a pharmacy increases the weight maintenance prognosis for dieters.
Now or never
According the the Royal Pharmaceutical Society, it is ‘Now or Never’. “Pharmacists need to become first and foremost providers of patient care, rather than dispensers and suppliers of medicines This is central to securing a future in which the profession can flourish,” it says.
To be a ‘Today’s Pharmacist’ and have your pharmacy remain a valued destination on the high street, start developing and promoting your one-on-one services now. For patients to recognise and value your services, use your consultation room for patient services and not storage space. Be properly equipped for a weight management service by having weighing scales comparable to the ones we provide, that can weigh patients up to 32 stone. Have a chair in the consulting room with no arms that is strong enough to support an obese patient. Be professional, knowledgable, understanding and effective with your weight service.
The pharmacists of tomorrow will have a much greater opportunity to make use of their extensive pharmacy education, long after the vending machines have dominated the prescription business.
PDF Version: todayspharmacist
OBESITY PREVENTION AND TREATMENT ON THE HIGH STREET
S. N. Kreitzman Ph.D, R.Nutr.
Howard Foundation Research
Treating overweight, but not-yet-obese people, in pharmacy, is obesity prevention on the high street. There are over 30 million overweight and obese people in the United Kingdom. Since no one ever became obese without first being overweight, it is important to provide real help to people at this stage. It is much less problematic to help people who do not have a massive amount of weight to lose and who also do not yet have some of the serious medical consequences associated with excess weight.
Pharmacy has become the prime location for weight management in the UK and Ireland. With the NHS ‘Call to Action’, pharmacy professional bodies are urging pharmacists to make their voices heard and shout about the good they do in improving people’s health. Take weight management for example. Helping people lose weight is not just about making them feel good but is also about preventing major long-term health problems, such as type 2 diabetes. This point was very well illustrated in a recent article in GP magazine that reported a staggering sevenfold rise in insulin use in type 2 diabetes over a nine year period.
But it seems that it’s not just the NHS that needs to hear what pharmacy has to say. The public do too. North London LPC was inundated with enquiries about a newsletter it had produced raising awareness of pharmacy services in the area.
So what does that mean to you as a pharmacist with a team already offering an established weight management service? Promote your service far and wide and show the public and the NHS what you’ve been doing to improve the health of the nation.
Fin McCaul, for example, is first and foremost a community pharmacist practicing in Manchester. He is also the Chairman of the Independent Pharmacy Federation and works for Bury CCG one day per week as its Long Term Conditions Lead.
Fin’s passion for independent pharmacy is second only to helping patients lose weight and stop smoking. With an average of 100 quits per year and well over 1000 patients helped through the weight loss service in his pharmacy, there is nobody better placed to talk about the opportunities and challenges for pharmacy now that Public Health commissioning has moved into the care of Local Authorities.
Delegation, motivation and marketing skills and advice for pharmacists and their team are just some of the benefits from his Stop Smoking/Weight loss clinics. At the 2013 Pharmacy show he organised a series of Patient Services Workshops delivered by Pharmacists who are successfully running weight services in their local community and want to share their knowledge and expertise.
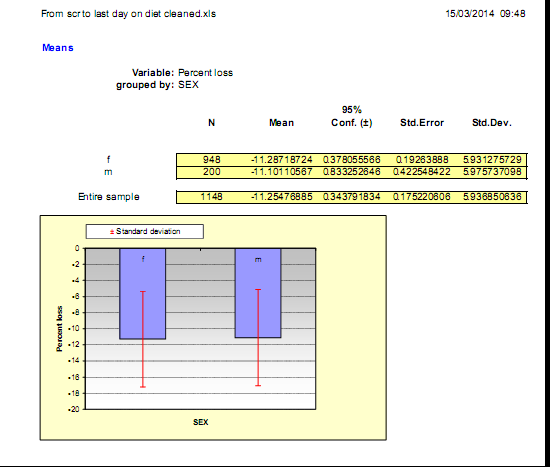
Fin’s expertise and results are not just anecdotes. He, along with many of the pharmacies treating overweight and obesity are generating extensive audit data from their weight management services. Results from one of his pharmacy audits below show the percentage of initial weight lost by over 1100 of his patients.
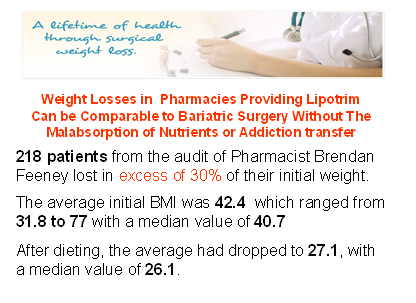
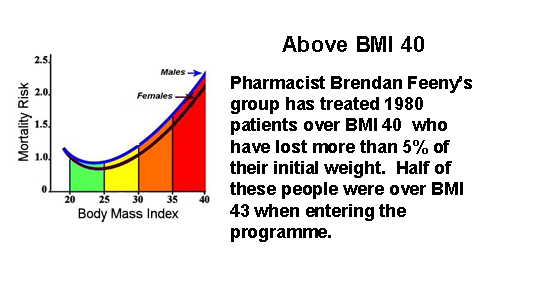
Pharmacy is an excellent provider of weight services for the community. Many overweight people in the BMI 25-30 range take advantage of pharmacy weight loss programmes recognising that they really work and confident that they are being monitored by healthcare professionals. Pharmacists’ expertise in weight management, however has proven extremely valuable for the treatment of obese and even the morbidly obese people. This is a group who could have qualified for bariatric surgery at great expense, risk and often compromised future life.
Effective weight loss absolutely needs to be monitored by knowledgeable healthcare professionals, because real weight loss is not benign. Type 2 diabetics, for example, who lose weight by compliance with a total food replacement diet programme, will induce remission of their diabetes within a few days and therefore continuing with hypoglycaemic medication can get them into serious difficulty. There are multitudes of patients taking medications such as warfarin or lithium, drugs which have a very narrow safety spectrum. Dieting can alter the absorption rate for these drugs so these patients need their dosages to be carefully monitored. There are some people who really should not be dieting at all. Pregnant women, patients with a recent history of surgery, stroke or heart attack are not logical candidates for weight loss. Effective weight loss should not be left to amateurs or internet sales. Healthcare professionals are needed, especially in pharmacy where continuous care can be provided even after the weight is lost, because weight maintenance requires the greatest attention and is not usually possible in a busy medical practice and appears to be almost impossible without professional help.
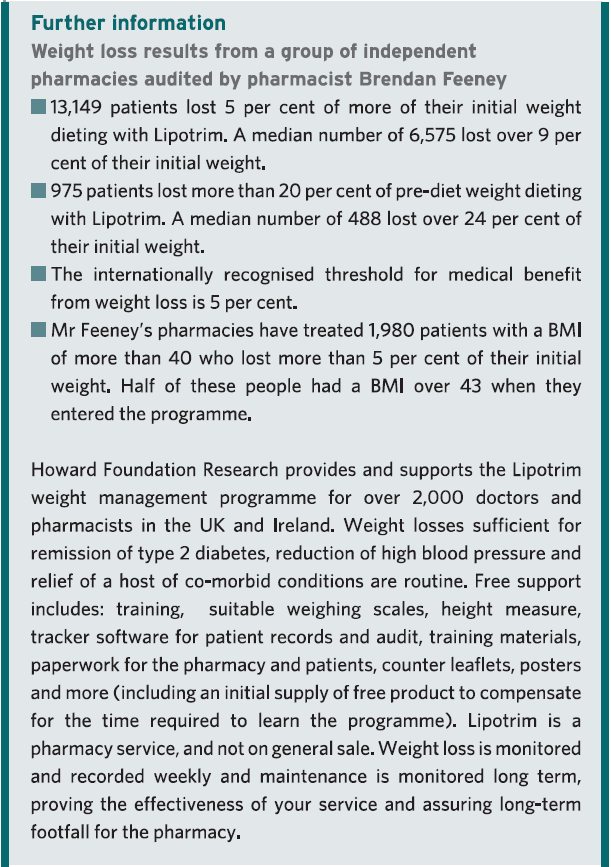
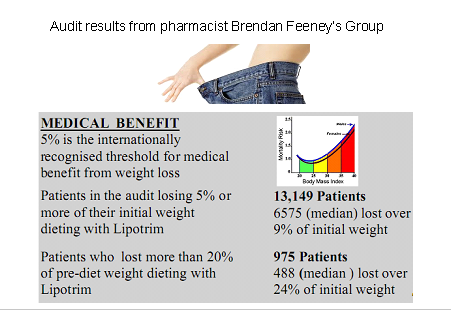
Although it is traditional to show successful dieters proudly occupying trousers which are now several sizes too large, there isn’t enough space to print over 13,000 examples. Results from this single audit of a group of pharmacies out of a collection of more than 2000 UK and Irish pharmacies currently treating overweight and obesity, is a vivid demonstration of the evidence base being accumulated for this absolutely essential community service from pharmacy.
Pharmacy is the only reliable community service providing and documenting long term weight management without the need major research grants or health service funding. Although there has been widespread press coverage for a £2.4 million grant by Diabetes UK to attempt to demonstrate that type 2 diabetes can be put into remission by effective weight loss, a fact that has been repeatedly reported in the medical press for over 30 years, pharmacies have been quietly and routinely succeeding with diabetes prevention and remission in their high street branches. Unlike bariatric surgeons, who need to justify the cost and risk of providing weight loss by surgical means on the basis of the phenomenal cost savings on the treatment of diabetes alone, weight loss in the pharmacy can accomplish the same results without massive expense and risk. And since total food replacement methods remove the substances of abuse for prolonged periods of time from those who may be suffering from a dopamine response to eating excess in their nucleus accombans , they don’t show the common addiction transfer syndrome that seems to be so common after bariatric surgery.
While activists continue to bellow about the size of soft drink containers, pharmacists are demonstrating how much their education and skills can be amplified by the convenience of access on the high streets of the UK. Pharmacy stands alone among the healthcare professionals in providing fantastic public health services such as smoking cessation, weight management, diabetes recognition, prevention and even treatment, medicines review, hypertension assessment and a host of other essential services very much needed in the real world. A major thank you is overdue.
PFD version: OBESITY-PREVENTION-AND-TREATMENT-ON-THE-HIGH-STREET
Recognising and managing addiction transfer
Jan 2013
Food addiction, according to Dr Nora Volkow, head of the National Institute for Drug Abuse, shares the same brain dopamine reward pathways as addictions to drugs and alcohol. It explains much of the compulsive overeating that results in obesity. The two treatments most likely to combat the excess weight of obesity are bariatric surgery and Lipotrim.
Bariatric surgery has been linked to many reports of addiction transfer – where after treatment the addiction to food transfers to
other substances or habits, such as alcohol, drugs and cigarettes. A recent study in the Archives of Surgery found a 50 percent rise in the frequency of substance abuse two years after the procedure.
Alcohol misuse, smoking cessation and weight management are high on the public health agenda and are areas that pharmacy is long familiar with. In fact, the addiction transfer from cigarettes to food is familiar and one that pharmacists counsel on when running a quit smoking service. Food addiction is therefore a subject that pharmacists should be advising on when offering a weight management service.
Drugs and food addictions activate the common dopamine reward pathway in the brain. The best treatment for addictions is complete abstinence from the addictive substance. With food this is not usually possible which is what makes dieting hard. Total Food Replacement diets, such as Lipotrim overcome this because people whose weight gain is due to food ‘abuse’ can safely avoid food until the habit is broken and normal eating habits can be re-introduced, for example in conjunction with the Lipotrim maintenance formulas.
PDF version: ICP LIPOTRIM COLUMN Jan 13
Positioning pharmacy as an effective option to bariatric surgery
Nov 2012
Recent NHS figures show that the number of people undergoing bariatric surgery has quadrupled in the last 5 years – from 1,573
people in 2006-07 to 6,723 in 2011-12.
Although bariatric surgery is very effective at producing rapid weight loss that causes type 2 diabetes to go into remission, it comes with a multitude of problems including high morbidity and mortality risk, prohibitive initial and followup costs and limited availability. However, there is a readily available alternative to bariatric surgery that is evidence-based, safer, much
more cost-effective and one where pharmacies are playing an active part: Very Low Calorie Diets (VLCDs) properly monitored by healthcare professionals.
The rise in bariatric surgery has led to prominent pharmacy figures Mike Holden, chief executive of NPA, and Ajit Malhi, AAH
Pharmaceuticals’ head of marketing services, arguing the case for pharmacy which is playing an increasingly prominent role in tackling obesity in the community, as part of the public health and Healthy Living Pharmacy drive.
With over 2000 pharmacies offering the Lipotrim VLCD programme, overweight people have ready access to a pharmacist who can not only help them reduce weight, but also assist them adopt healthier lifestyles, change eating and exercise habits and pre-empt or control existing diabetes.
Pharmacists therefore deserve considerable recognition for providing a service capable of promoting remission of type 2 diabetes and relief of co-morbidities, where present, without depleting the assets of the NHS. And, crucially, praise for the effective reatment of excess weight in hundreds of thousands of patients, where documentation of weight loss represents evidence for the value of pharmacy.
PDF version: ICP LIPOTRIM COLUMN Nov_ r2
GP/PHARMACIST: SYNERGY FOR OBESITY CONTROL
In order for weight loss programmes to be successful, it is essential to conduct post-diet monitoring and provide the overweight patient with long-term support. The Lipotrim pharmacy-based programme, therefore, encourages an interactive approach with GPs to ensure successful, sustained weight management
it seems easy to justify practice time and resources to assist overweight and obese patients lose weight. The link to type 2 diabetes alone is sufficient. With rapid weight loss, normalisation of blood sugar levels is achieved in days. With further weight loss, the disease can be held in remission.
Better long-term glycaemic control is achieved with rapid weight loss, even after some weight regain, than is achieved by losing the same amount of weight more slowly. Almost 50% of hypertensive patients can reduce drug treatments with weight loss. Surgical interventions can be scheduled when substantial weight is lost. Fewer antidepressants are required and overall, the frequency of GP visits is significantly lower for leaner patients.
There is no shortage of choice to meet the weight loss needs of individual patients: drugs, both current and promised for the future; dietetic referral; exercise on prescription and pharmacy-based treatment programmes. Each has a place depending upon the specific clinical needs of the patient. An exercise prescription may not be the best choice for a 40-stone patient who may struggle simply to walk, which at this weight is considerable exercise.
While willpower can often help people lose weight over a short defined period, upholding control for the months, years or even decades required for maintenance is quite a different story. Loss of weight by any means confers absolutely no lasting legacy for weight maintenance. Weight loss, however achieved, is only the beginning of the treatment, not the end point. When the drug therapy is discontinued, when the counsellor moves on, when the patient is “cured” of excess weight – this is the point at which a dieter requires the maximum attention and assistance.
Weight management requires control of eating behaviour over a sustained period of time. A difficulty comes with justifying practice time and resources for a patient who has achieved weight loss and is now both healthier and at a normal weight. The expectation that this patient will sustain the weight loss without considerable help is naïve.
Lipotrim pharmacy-based programmes are ideal for the varying weight management needs of patients. Obesity prevention is part of the pharmacy complement of health promotion services, dealing with excess weight before it reaches obese levels and exacerbates comorbidities. The care of patients during weight loss is advantageous when monitored by the pharmacist, who understands the implications of other drug treatments that may interact with the weight-loss programme. But it is at the post-diet stage that the pharmacist is best equipped to provide essential long-range guidance, support and education that will increase the length of time that the weight loss is maintained.
Both the new GP and the pharmacy contracts strongly encourage interactive efforts to deal with a range of health problems, most of which have weight-related implications. Weight loss is vital for management of cholesterol, blood lipids, diabetes, hypertension and asthma. It even impacts upon programmes for smoking cessation. The success of the Lipotrim pharmacy-based programmes in dealing with weight loss and maintenance should not be overlooked.
PDF version: 5-5-synergy
PHARMACIES LEAD THE WAY IN OBESITY MANAGEMENT
Pharmacists can play an important role in weight management.
And there’s evidence to support their effectiveness.
Early in October 2010, the National Obesity Forum Conference in London heard a presentation by Fin McCaul, the pharmacist at Prestwich Pharmacy in Manchester. Mr McCaul, who is also chair of the Independent Pharmacy Federation, was presenting his pharmacy’s outstanding results in treating overweight and obesity at the pharmacy. His paper, ‘Options for the orbidly obese’, was based on 1,148 overweight patients with a median initial BMI of 33.6 kg/m2
enrolled into the Lipotrim weight management programme. Of these patients, 25 per cent were morbidly obese with a BMI >40 kg/m2. At the time of audit, during which many patients were still actively dieting, the median BMI had decreased to <30 kg/m2. Results showed that 94 per cent of the dieters lost more than 5 per cent of their pre-diet weight, 47 per cent lost more than 10 per cent, and 21 per cent of the patients lost more than 20 per cent. The presentation highlighted the impressive weight loss results being achieved in pharmacy. Given that the organisers of the programme chose to position the presentation in the section of the conference devoted to bariatric surgery, Mr McCaul concentrated his results on the subset of the dieters who were of greatest relevance to the surgeons – the morbidly obese. Morbidly obese people are generally considered ‘heart sink’ cases; they are notoriously difficult to treat. The reason is largely due to the common chemistry with other examples of substance abuse. Recognition of this common chemistry is now leading to the development of weight management strategies involving drugs which are important in the treatment of alcohol and drug addictions.
 Advantages of weight loss
Advantages of weight loss
There is certainly plenty of justification for helping overweight patients. Weight loss can lower blood pressure, normalise blood lipids, practically eliminate type 2 diabetes, reduce the severity of asthma, bring relief to arthritics, increase the fertility of women hoping for pregnancy, relieve sleep apnoea, and provide an opportunity for patients to be considered for Pharmacists can play an important role in weight management. And there’s evidence to support their effectiveness. elective surgery. Loss of weight can decrease the need for antidepressants, make exercise more possible – thus improving cardiovascular health, and can vastly improve the quality of life for patients. Methods of treatment, however, are not universally agreed upon. Somewhat unsurprisingly, bariatric surgeons tend to favour the surgical approach to weight loss. According to the Department of Bariatric Surgery at Imperial College, the current burden of morbid obesity in the UK is approximately 720,000 patients who meet NICE criteria for eligibility for surgery. In 2008 only 4,000 operations for morbid obesity were performed in the public and private sector combined. Even if the number of patients being treated by surgery was doubled, the impact on the problem would still be small and fall far short of the treatment needs of the seriously overweight population. Most surveys estimate that in the UK about 60 per cent of the population are overweight and about 30 per cent are already obese. Assuming a 60 million UK population, the number of people with a weight problem calculates to 36 million overweight and 18 million obese. Treating this many people surgically is unrealistic, to say the least. In addition, there is an increasing tendency for people to seek less expensive or more readily available bariatric surgery abroad, which has led to an ethical dilemma for NHS specialists. The costs to the NHS of providing aftercare, expected free by UK citizens, or emergency subsequent surgery when procedures initiated abroad go wrong, can be unplanned for and a substantial drain on NHS resources2.
Pharmacists’ role
Bariatric surgeons (in the current absence of a selection of effective weight loss drugs) are increasingly attempting to convince the public and the professionals that surgery is the only method of effectively treating seriously overweight people. The evidence presented by Mr McCaul clearly demonstrated that there is a non-invasive treatment that can be as effective. Like the claims for remission of diabetes as a result of the surgery, diabetes remissions are obtained by pharmacists as well since it is the loss of weight that leads to the remission. Usually, the blood sugar control is so rapid that it has become mandatory to get the doctor’s cooperation in stopping oral hypoglycaemic medications prior to the patient dieting. Without this step, patients are not permitted to participate in the Lipotrim programme. The results presented for this difficult cohort of morbidly obese patients was suitably impressive. These were very large individuals indeed, with half presenting with a BMI above 45 – the heaviest just below BMI 70. From this subset of 267 patients, the results reported were:
- Median BMI was 45.1 at enrolment;
- 237 patients lost over 5 per cent of pre-diet weight;
- 141 had lost over 10 per cent of pre-diet weight;
- 34 patients had lost over 20 per cent.
The programme at Prestwich is only one of more than 1,500 UK pharmacies treating overweight patients in this way. What’s more, the introduction of Lipotrim’s patient tracker software now permits on-demand audits of the results obtained by each pharmacy – essential for demonstrating effectiveness for commissioning requirements. Mr McCaul’s audience – primarily surgeons – listened for the most part in attentive silence, but the questions put to him at the end of his presentation were extremely revealing and illuminating. One overly distressed questioner was seriously worried that a few weeks of what is essentially a nutrientcomplete enteral feed (to effectively treat morbid obesity and its medical consequences) would compromise the patient’s relationship with food and cause chaos in the family dynamic. As she summed it up: there was a risk of “demonising food”. Leaving aside for a moment the point that bariatric surgery is an invasive and dangerous procedure that results in a state of permanent malnutrition, it is worth remembering that morbidly obese individuals generally have a very destructive relationship with food. To these individuals, food is a substance of obsession and addiction, and eating is a compulsive behaviour. Modifying the patient’s relationship with food is arguably a very worthwhile goal.
One of the more disturbing post-surgical problems (being widely reported from the US, where large numbers of surgeries are performed) is the unexpected and unwelcome problem of addiction transfer. A quick Google search unearths the massive scope of the problem, in which the loss of the ability to eat (due to weight loss surgery) is apparently leading to the development of substitute addictions – to alcohol, drugs and other destructive activities.
 Total food replacement
Total food replacement
The total food replacement programme owes its success in no small part to the first principle that – instead of inducing malnutrition – the formulated enteral feeds are generally much more nutritious than the ordinary food choices of the
patients. As all essential nutrients are provided, the patients remain healthy throughout their programme. Where there
is a component of food abuse associated with the weight problem, the nutrient formulas are the only way that normal
foods – the addictive substances – can be safely eliminated so that the dieter can have a better chance of success.
An expanding network of pharmacists is offering a range of treatments for weight problems. Pharmacists have the training, the respect of the public, the contact hours and the desire to offer weight management as a professional service.
The National Institute for Health and Clinical Excellence (NICE) recommends that specialists be used for extended treatments involving total food replacement. Pharmacists that join this programme are trained and experienced specialists in this area.
Unlike surgery, there is no cost to the NHS, and no serious sideeffects.
The cost to the patient is less than the money a morbidly obese individual will have been spending on food, and the level of weight loss is sufficient to put type 2 diabetes into remission. The documented and audited successes of these dieters is a welcome testament to the leadership role that pharmacists are taking by providing important healthcare services to their community
PDF version: 1-6-pharmacist