S. N. Kreitzman Ph.D, R.Nutr.
Howard Foundation Research
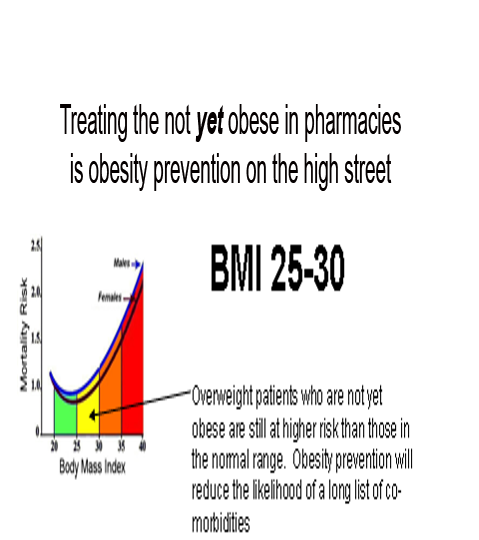
Treating overweight, but not-yet-obese people, in pharmacy, is obesity prevention on the high street. There are over 30 million overweight and obese people in the United Kingdom. Since no one ever became obese without first being overweight, it is important to provide real help to people at this stage. It is much less problematic to help people who do not have a massive amount of weight to lose and who also do not yet have some of the serious medical consequences associated with excess weight.
Pharmacy has become the prime location for weight management in the UK and Ireland. With the NHS ‘Call to Action’, pharmacy professional bodies are urging pharmacists to make their voices heard and shout about the good they do in improving people’s health. Take weight management for example. Helping people lose weight is not just about making them feel good but is also about preventing major long-term health problems, such as type 2 diabetes. This point was very well illustrated in a recent article in GP magazine that reported a staggering sevenfold rise in insulin use in type 2 diabetes over a nine year period.
But it seems that it’s not just the NHS that needs to hear what pharmacy has to say. The public do too. North London LPC was inundated with enquiries about a newsletter it had produced raising awareness of pharmacy services in the area.
So what does that mean to you as a pharmacist with a team already offering an established weight management service? Promote your service far and wide and show the public and the NHS what you’ve been doing to improve the health of the nation.
Fin McCaul, for example, is first and foremost a community pharmacist practicing in Manchester. He is also the Chairman of the Independent Pharmacy Federation and works for Bury CCG one day per week as its Long Term Conditions Lead.
Fin’s passion for independent pharmacy is second only to helping patients lose weight and stop smoking. With an average of 100 quits per year and well over 1000 patients helped through the weight loss service in his pharmacy, there is nobody better placed to talk about the opportunities and challenges for pharmacy now that Public Health commissioning has moved into the care of Local Authorities.
Delegation, motivation and marketing skills and advice for pharmacists and their team are just some of the benefits from his Stop Smoking/Weight loss clinics. At the 2013 Pharmacy show he organised a series of Patient Services Workshops delivered by Pharmacists who are successfully running weight services in their local community and want to share their knowledge and expertise.
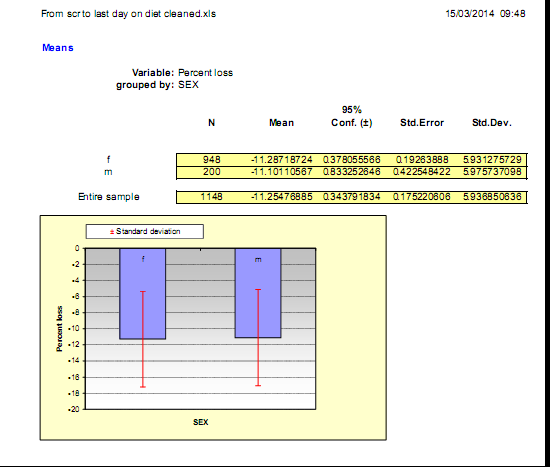
Fin’s expertise and results are not just anecdotes. He, along with many of the pharmacies treating overweight and obesity are generating extensive audit data from their weight management services. Results from one of his pharmacy audits below show the percentage of initial weight lost by over 1100 of his patients.
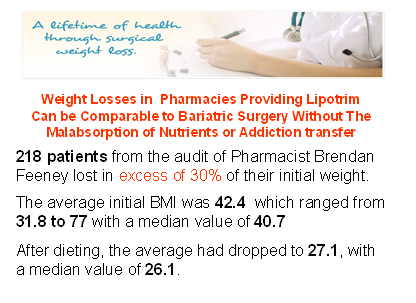
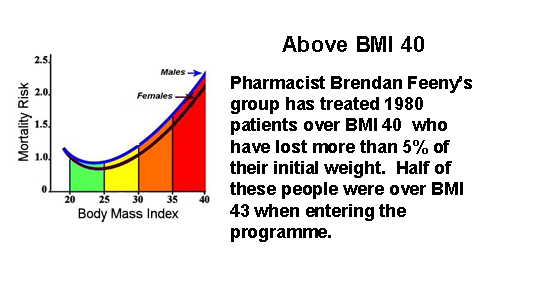
Pharmacy is an excellent provider of weight services for the community. Many overweight people in the BMI 25-30 range take advantage of pharmacy weight loss programmes recognising that they really work and confident that they are being monitored by healthcare professionals. Pharmacists’ expertise in weight management, however has proven extremely valuable for the treatment of obese and even the morbidly obese people. This is a group who could have qualified for bariatric surgery at great expense, risk and often compromised future life.
Effective weight loss absolutely needs to be monitored by knowledgeable healthcare professionals, because real weight loss is not benign. Type 2 diabetics, for example, who lose weight by compliance with a total food replacement diet programme, will induce remission of their diabetes within a few days and therefore continuing with hypoglycaemic medication can get them into serious difficulty. There are multitudes of patients taking medications such as warfarin or lithium, drugs which have a very narrow safety spectrum. Dieting can alter the absorption rate for these drugs so these patients need their dosages to be carefully monitored. There are some people who really should not be dieting at all. Pregnant women, patients with a recent history of surgery, stroke or heart attack are not logical candidates for weight loss. Effective weight loss should not be left to amateurs or internet sales. Healthcare professionals are needed, especially in pharmacy where continuous care can be provided even after the weight is lost, because weight maintenance requires the greatest attention and is not usually possible in a busy medical practice and appears to be almost impossible without professional help.
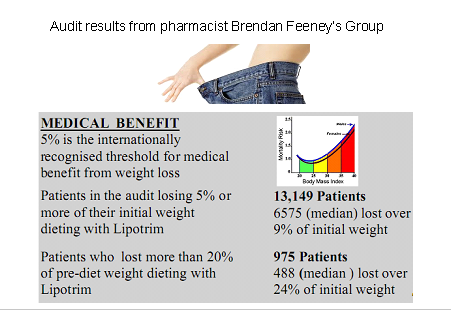
Although it is traditional to show successful dieters proudly occupying trousers which are now several sizes too large, there isn’t enough space to print over 13,000 examples. Results from this single audit of a group of pharmacies out of a collection of more than 2000 UK and Irish pharmacies currently treating overweight and obesity, is a vivid demonstration of the evidence base being accumulated for this absolutely essential community service from pharmacy.
Pharmacy is the only reliable community service providing and documenting long term weight management without the need major research grants or health service funding. Although there has been widespread press coverage for a £2.4 million grant by Diabetes UK to attempt to demonstrate that type 2 diabetes can be put into remission by effective weight loss, a fact that has been repeatedly reported in the medical press for over 30 years, pharmacies have been quietly and routinely succeeding with diabetes prevention and remission in their high street branches. Unlike bariatric surgeons, who need to justify the cost and risk of providing weight loss by surgical means on the basis of the phenomenal cost savings on the treatment of diabetes alone, weight loss in the pharmacy can accomplish the same results without massive expense and risk. And since total food replacement methods remove the substances of abuse for prolonged periods of time from those who may be suffering from a dopamine response to eating excess in their nucleus accombans , they don’t show the common addiction transfer syndrome that seems to be so common after bariatric surgery.
While activists continue to bellow about the size of soft drink containers, pharmacists are demonstrating how much their education and skills can be amplified by the convenience of access on the high streets of the UK. Pharmacy stands alone among the healthcare professionals in providing fantastic public health services such as smoking cessation, weight management, diabetes recognition, prevention and even treatment, medicines review, hypertension assessment and a host of other essential services very much needed in the real world. A major thank you is overdue.
PFD version: OBESITY-PREVENTION-AND-TREATMENT-ON-THE-HIGH-STREET