S.N Kreitzman Ph.D, R.Nutr. (UK Registered Nutritionist), & V. Beeson Howard Foundation Research Ltd. Cambridge UK
It is widely understood that weight loss, weight gain or weight maintenance is determined by the relationship between Calories eaten compared with Calories used. For each individual, with unique genetics and distinctive lifestyles, it makes sense that the Calorie balance point will differ between people – along with individual differences in almost every other aspect of life. Yet we are expected to take the values of 2000 Calories a day for women and 2500 Calories a day for men as fixed balance points and when reality proves different we are expected to censure the individual.
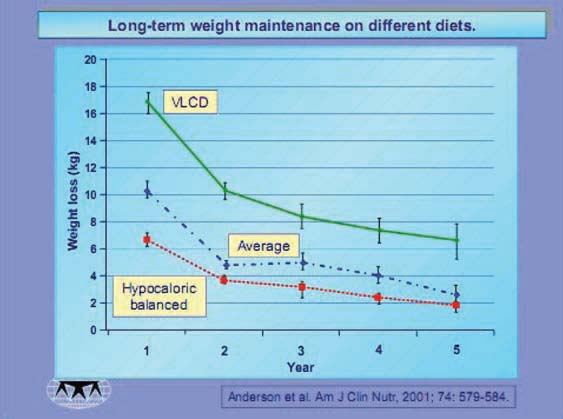
The true energy balance level – the Calorie intake level that will provide for weight maintenance rather than gain or loss
for an individual, is a very important piece of information. Weight maintenance is the most difficult aspect of weight control and without an accurate determination of the critical equilibrium Calorie level, people must rely on guesswork. A successful outcome becomes very unlikely.
Measuring the energy expended by people living normal lives is almost impossible. There are techniques using double isotope labelledwater, which are extremely expensive and virtually never used. Fortunately, whatever the energy levels used by individuals, they are surprisingly consistent. The reason for this is that despite the unrealistic claims for a massive Calorie usage with exercise equipment, the reality is much more depressing. A mile run uses about 100 extra Calories, not far from the contribution provided by a sports drink. Using up a pound of body fat, however, requires a deficit of 3500 calories. Few seriously overweight people have the capacity to run the 35 miles it takes to lose an extra
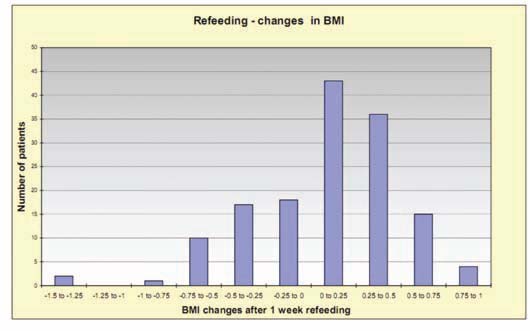
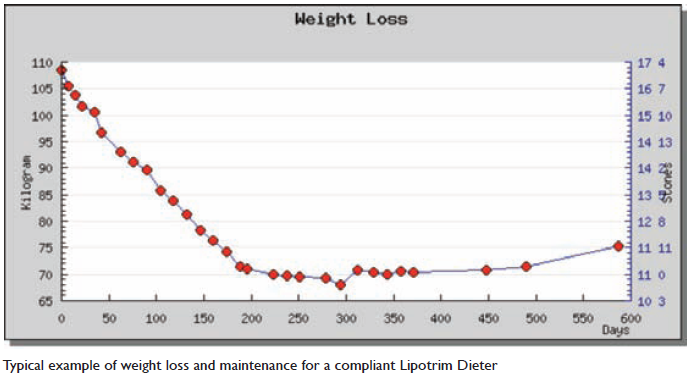
pound of fat weight. So, Calories used each day for most people are remarkably consistant. What about intake? Under most conditions it is extremely difficult to measure actual daily intake. There has been, however, an exciting benefit from the auditing of weight loss results with dieters using the Lipotrim pharmacy service. The vast majority of compliant dieters S.N Kreitzman Ph.D, R.Nutr. (UK Registered Nutritionist), & V. Beeson Howard Foundation Research Ltd. Cambridge UK haveweight loss experiences that follow the pattern seen in the case shown here. Many pharmacies have hundreds of such cases. It should be obvious that the weight loss over a fixed time is virtually the same, week after week. This must mean that essentially the same amount of fat is being depleted every day, and since the Calories provided
by the Lipotrim diet formulas are constant, the calories the body must provide to make up the difference between the amount eaten and the amount used (defined as dieting) must be about the same every day
 .
.
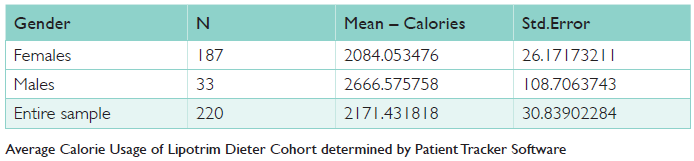
The patient record keeping and audit tool, the Lipotrim Patient Tracker, used by many pharmacies running the service
has now been augmented to display the Calories used by each compliant dieter. Assessing the Calories used per day by
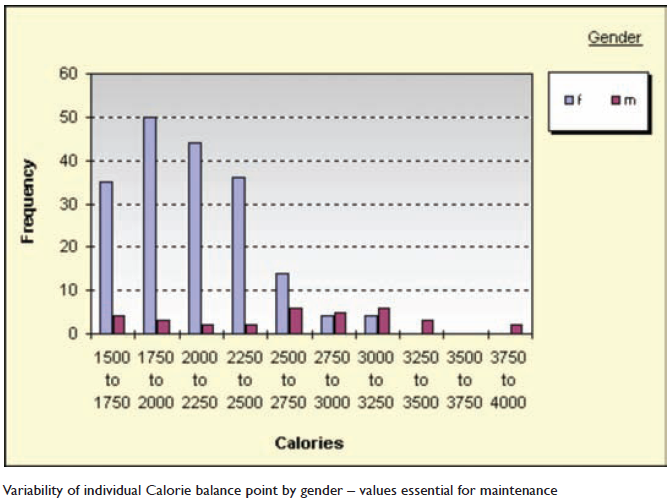
220 dieters treated by pharmacist, Gareth Evans, yielded on average 2171 Calories, however comparing the 187 females with the 33 males in the sample yielded an average Calorie usage of 2084 for women and 2666 for men. Quite realistic averages. The reality, however, for individuals can be considerably different from the group averages. The graph below shows the actual distribution of equilibrium Calories. Thirty one percent of the women had Calorie expenditures above 2000 and forty five percent had values below 2000 – some far below. These people will have vastly different maintenance experiences if they adhere to a 2000 Calorie a day maintenance regime. While there are fewer men in the sample, it is clear that there is a substantial spread in the individual values and about 33% of this cohort are below the 2500 classic value. There is yet another critically important consequence of identifying the equilibrium value for Calorie intake that determines whether there will be maintenance, gain or loss. There have been articles in the press in recent months suggesting that weight lossis trivially easy. The notion that cutting out a piece of toast a day (about 80 Calories) if
done every day will result in a loss of over 8 pounds in a year can not be valid because seriously overweight and obese people are not eating at the equilibrium intake. Yes it would be true for an individual with a personal maintenance level of 2000 Calories and who was consistently eating at that level to lose weight by cutting 80 Calories a day out of their daily intake. It is unrealistic to think that a seriously overweight person is habitually eating 2000 calories a day. Eating 80 calories less than the typical, 3000 Calories (pick a different excessive number if you don’t like 3000) will only slow the weight gain a bit. The application of the Patient Tracker software is advancing the understanding of weight loss and maintenance of real people and also documenting the substantial impact on the management of weight related medical problems such as type 2 diabetes and hypertension. It is also providing valuable data which is satisfying the need for evidence based treatment.
PDF version: 2-7-napc-calorie-balance-point