contrasting very low calorie diets against bariatric surgery
S.N Kreitzman, V. Beeson & S.A Kreitzman
Interest in the use of weight loss to treat type 2 diabetes has intensified in recent years, despite the fact that the rapid therapeutic effect of weight loss on type 2 diabetes has been well known for decades and largely ignored. The renewed interest can be attributed in large part, to a number of publications generated by evidence from bariatric surgery, of the almost universal prompt remission of diabetes with weight loss after successful surgery.
One such study was published in the Journal of Endocrinology and Metabolism in 2004 by Cummings et al “Gastric Bypass for Obesity: Mechanisms of Weight Loss and Diabetes Remission”. In support of their efforts to promote the use of surgical techniques, the authors claimed that no more than 5‐10% of body weight can be lost through dieting, exercise or the few available anti‐ obesity medications. They further write ‐ correctly ‐ that
“Importantly, even mild weight loss confers disproportionate health benefits, in terms of ameliorating obesity‐related co‐morbidities. Nevertheless more substantial and durable weight reduction would improve these ailments more effectively”
…and not correctly that “At present, bariatric surgery is the most effective method to achieve major weight loss. The best operations reduce body weight by 35‐40%.”
Quite a dramatic claim, but surgery is not the only effective means of achieving this amount of weight loss when it is necessary.
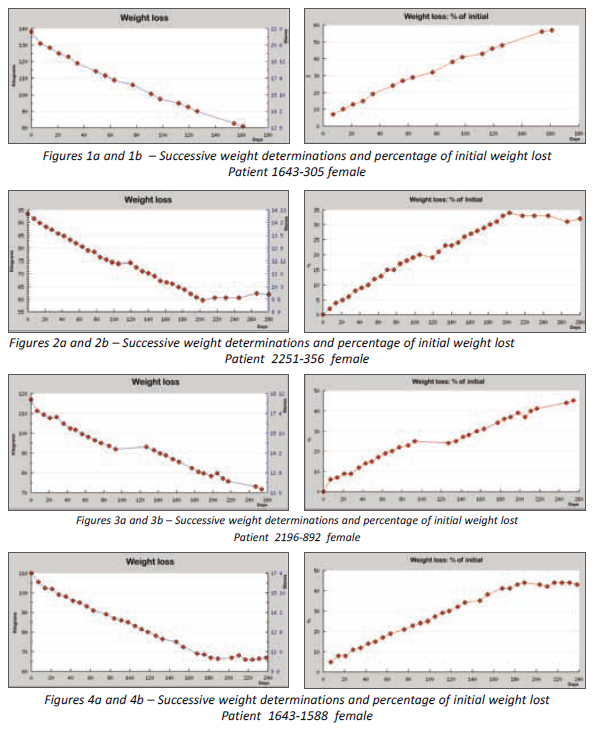
There is a readily available alternative to bariatric surgery, without the problematic aspects of bariatric surgery: high morbidity and mortality risk, prohibitively high cost, possible post operative addiction transfer and in consideration of the large numbers of severely overweight people with or without diabetes, extremely limited availability. This alternative is the very low calorie diet. Detailed records have been kept of the weight loss results of every person who has dieted with Lipotrim either at a UK GP practice, hospital clinic or pharmacy for the past 26 years, however, the availability of computer software to replace paper records has made auditing of the results far more practical. Using audit data, accumulated from UK pharmacies, it was easy to identify cases of successful weight losses in excess of 35%. There are many very high weight patients being treated at pharmacy. A recent audit of patients attending a single pharmacy, Prestwich pharmacy in Manchester, had 270 successful patients with initial BMIs in excess of 40. And there are currently over 2000 pharmacies running the service in the UK. Four recent cases will be presented in this report. It has to be emphasised that these people, although at higher BMI than many of the people treated in pharmacy, were participating in the routine Lipotrim weight loss service in pharmacy and the total cost to each was £36 per week.
These four patients did not happen to suffer from diabetes, although many of the people being treated by the pharmacies did present with type 2 diabetes and achieved rapid remission. As has already been recognised, however, this magnitude of weight loss is not necessary for rapid
remission of the diabetes. Most type 2 diabetics show normal blood sugars within the first week of dieting. The selection of these examples is simply evidence to contrast the achievements of VLCD use with the weight losses achieved by surgery. The four women whose initial weight ranged from 14 stone 10 pounds (93.5 kg) to 20 stone 9 pounds (131 kg) collectively lost 25 stone 12 pounds (164.1 kg) . BMI at the start averaged 43 and ranged from 35 to 49.. Following weight loss their average BMI was 27 and ranged from 23 to 31. The percentage of initial weight lost ranged from 35 to 39%. Plots of the weight changes for the 4 cases are presented in Figures 1‐4 This pharmacy weight loss programme is based upon a replacement of all normal foods with a nutrient complete formula. There are many advantages to this approach, especially with severely overweight people. There is now an expanding literature based upon numerous addiction investigations, which demonstrate that in a high percentage of high BMI people, the same metabolic pathways that are generally recognised as part of the addiction profile are shared by people who are using food as a substance of abuse. In the case of every known addiction, it is absolutely necessary to completely stop the abused substance. This is difficult when the substance is alcohol, tobacco or drugs, it is unachievable when the addiction is to food. Food is required in order to stay alive. While ultimately food is required for energy, there is no shortage of energy stored as fat and glycogen in overweight people. What must be supplied in order to keep people healthy are the vitamins, minerals, trace elements essential amino acids and essential fatty acids. Depletion of any of these nutrients will compromise health. Use of a nutrient complete formula provides all the essential nutrients in the absolute minimum number of calories. This allows weight loss at the maximum safe rate, while allowing the person to completely stop eating the foods that they are abusing. This is the only approach that will interfere with the addictive problem and offer a reasonable chance of establishing a normal relationship with food in the future.
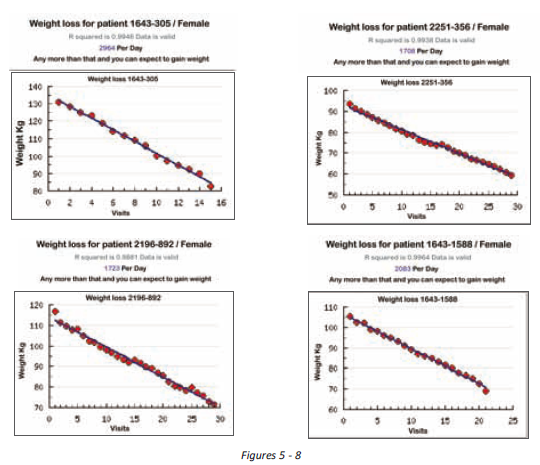
There is yet another important benefit to using a food formula instead of traditional foods. With ordinary foods which are derived from various plants and animals and which themselves will differ in nutrient composition and calorie contribution, it is not possible to get an accurate estimate of the energy intake.
Food composition tables present averages from a large number of samples and can differ widely from the composition of a specific sample.
The caloric composition of a defined formula can be known with considerable precision. Therefore dieters can know exactly the number of calories they are eating each day. It is well known that the calorie deficit required to lose a pound of body fat is fixed at 3500. The difference between the calories in the formula and the calories used by the individual based upon genetics and lifestyle will represent the rate at which the 3500 calories is being depleted. Calorie utilization for most people, especially severely overweight people who are not usually involved in massive exercise programmes, does not vary a great deal from day to day. Variations are trivial when it is realised that running a mile only consumes an additional 100 calories, therefore the calories used each day is basically constant. This explains the essentially straight line pattern of weight loss seen in each of the dieter’s weight loss graph. And from the daily changes in weight, it is easy to determine the number of calories used by each individual day after day. This, then will inform the individual of the critical calorie intake that will determine whether weight is gained, lost or maintained. There is no other method to gain this information under real life conditions.
The graphs in figures 5‐8 illustrate the determination of maintenance level intake for the 4 individuals. Cummings et al, in the paper cited above provide estimates of the cost of bariatric surgery (2004 data) represented as QALY (quality adjusted life years) ranging from $5,400 to $36,300 which they state is well under the $50,000 generally regarded in the United States as being cost effective. At £36 per week in 2012, it might be worth considering a VLCD pharmacy programme which will routinely provide weight losses of 1 stone (6.3 kg) a month for women and 1.5 stone (10 kg) for men. And the programme can be used with people who have far less weight to lose than the BMI 35‐40 subjects reported here. These programmes are suitable for obesity prevention in overweight, but not obese people BMI 25‐30. Far more appropriate a contribution to public health and of course prevention of diabetes.
S.N Kreitzman Ph.D, R.Nutr. (UK Registered Nutritionist), V. Beeson & S.A Kreitzman Howard Foundation Research Ltd. Cambridge UK