Marks and Schrijver
Reports on tasks
for scientific cooperation
(SCOOP)
Task
7.3 – Collection of data on products intended
for use in very-low-calorie diets.
Report September 2002
Reports
submitted on behalf of the VLCD European Industry Group to the SCOOP
working group on very-low calorie diets between 1998 and 2001, consolidated
2001.
by
John Marks
MA, MD, FRCP, FRCPath, FRCPsych Life Fellow, Girton College, Cambridge CB3 0JG
and
Jaap
Schrijver . Manager Corporate Regulatory Affairs for foods for particular
nutritional uses (PARNUTS) – Royal Numico NV
CONTENTS
INTRODUCTION
EXECUTIVE
SUMMARY & CONCLUSIONS
Summary
Conclusions
1.1`The prevalence of
excess weight
1.2
Excess weight and
morbidity
1.3
Weight increase and
mortality
1.4
The economic cost of
obesity
SECTION II THE
SAFETY OF VERY LOW CALORIE DIETS IN EXPERIMENTAL AND CLINICAL USE
2.1. The prime
data
2.1.1
Published monitored
studies
2.1.2
Experience in general
(mainly free sale) use
2.2
Putting the spectre of
liquid protein diets to rest
2.3
Clinical audits on safety of
VLCD
2.3.1
Specific
Audits
2.3.2
Investigation of reputed
deaths with nutrient complete VLCD
2.3.3
Audits on subjects with BMI
under 30
2.3.4
Audits on the prime
data
2.4
Special tests for
safety
2.4.1
Laboratory
studies
2.4.2
Electrocardiographic
evidence of cardiac integrity
2.5
Data on side
effects
2.5.1
General side
effects
2.5.2
Cholelithiasis
2.5.3
Bone density
2.5.4
Data on eating
disorders
2.6
Data on aspects of use and
control in practice
2.6.1
Resting metabolic rate
reduction during and after dieting
2.6.2
Relationship between diet
energy and rate of weight loss
2.6.3
Weight
cycling
2.6.4
Continuous versus
intermittent use
2.7
Long-term
efficacy
SECTION III
RECENT SCIENTIFIC STUDIES TO PRODUCE A BETTER UNDERSTANDING OF THE PROPERTIES OF
VLCD
3.1 Examination of body composition determination methods
3.1.1 Reliability of the analytical methods
3.1.2
Kjeldall method for nitrogen determination
3.1.3 Reliability
of indirect methods of estimating the body protein economy
3.1.4
Variation introduced by different formulae for indirect
determinations
3.1.5 Summary of the reliability of composition estimates
3.1.6
Significance of these variations to the Forbes/Prentice graphs
3.2 Re-examination
of old and examination of new data on body composition changes
3.2.1
Re-examination of the Forbes/Prentice graphs
3.2.2 The body
composition studies expressed in terms of BMI status
3.2.3 Body
composition studies expressed in terms of the energy value of the
diets
3.3 The Keys (1950)
Minnesota study – an appraisal
3.4 A
re-appraisal of the Forbes and Prentice graphs
3.5 Further data
relating to body composition study determination
3.6 Summary of the
body composition determinations
3.7 Submission
related to the matter of positive and negative nitrogen balances
3.8 Studies which
provide information on desirable carbohydrate level.
3.9Observations made after the circulation of
the first draft of the report to the working group.
SECTION IV.
MEDICAL AND SCIENTIFIC JUSTIFICATION FOR THE USE OF MODERN NUTRIENT COMPLETE
FORMULA DIETS WITH ENERGY VALUE LESS THAN 800KCALS PER DAY.
SECTION V.
HEALTH PRECAUTIONS FOR THE USE OF VLCD
5.1 Medical
precautions for the use of VLCD
5.2 Medical
supervision of individuals apparently healthy apart from excess
weight.
APPENDIX
1: TABLE OF THE PRIME DATA
APPENDIX II
BIBLIOGRAPHY FOR PRIME DATA AND OTHER DATA
APPENDIX III
DATA FOR THE BODY COMPOSITION EXAMINATION.
Introduction
When the SCOOP
Task 76.3 was first announced, the VLCD European Industry Group asked to submit
a report which had been prepared by one of us (JM) in March 1998. The SCOOP
Committee, during the first plenary meeting in Maastricht, The Netherlands on
March 15th and 16th 2000 accepted this report. A request
was made by the Committee that those sections of the report which were concerned
with scientific and medical data be updated to early 2000 and submitted as a
discussion paper for the next meeting. Subsequently a series of further papers
was requested by the Committee and submitted in the years 2000 and 2001 by JM
and JS.
The present
document which is referred to in the SCOOP Report to the EU Commission of August
2001 as Marks J and Schrijver J (2001) is the summation of all these reports
from March 2000 to July 2001. It has been edited to try to remove any overlap
resulting from the need, during the various meetings of the Committee to explain
the background to the further reports. In addition the information is not
presented in strict chronological order but in relation to the topics that were
covered.
Possible conflicts of
interest.
These original
documents were prepared by one or both of us as independent scientists and were
not discussed with the European VLCD Group. However members of that group were
very helpful in finding copies of overseas scientific papers not available in
United Kingdom libraries and in providing background data relating to their own
studies.
Neither of us is
currently employed by any of the member companies of the European VLCD Group
though John Marks has, in the past received a fee as Consultant to Cambridge
Nutrition Ltd.. Over the period of the preparation of this report John Marks has
been a Life Fellow of Girton College, Cambridge.
Jaap Schrijver has his
expertise in biochemistry and nutrition. He is employed by Royal Numico NV since
1991. He holds the position of Manager Corporate Regulatory Affairs for foods
for particular nutritional uses (PARNUTS). These foods include VLCD products
although the company has currently not an interest in these products. As a
representative of the Dutch association for PARNUTS foods, he participates in
the regulatory activities of the Association of the Food Industries for PARNUTS
(IDACE). The IDACE secretariat has its office in Paris.
Acknowledgement
I want to express my particular thanks to Dr Stephen Kreitzman and Valerie
Beeson of Howard Foundation Research Ltd. (Lipotrim), who undertook a substantial
proportion of the original research on which Section III, the ‘Recent Scientific
Studies’ is based. Not only did they make available to us copies of the
published work, but also shared with us much of the basic data so that we could
convince ourselves that their results, which demonstrated substantial
misunderstanding in much published metabolic work, could be thoroughly checked.
On the basis of this, we were not only able to confirm the validity of the
Kreitzman and Beeson studies, but from their bibliographies undertake
cross checks of the errors or omission in the earlier work.
We want to make it quite clear that we found no evidence of deliberate
distortion or deliberate misinterpretation in the early works. Most of
the errors occurred because the biological scientists did not fully understand
the assumptions involved, exactly what their indirect methods of
determination meant or the extraneous factors that influenced their results
and interpretations.
EXECUTIVE SUMMARY &
CONCLUSIONS
Preamble
This report presents evidence for VLCDs
collected since the Scientific Committee for Foods Report of 1990.
In 1990 the SCF Report was based largely
on the experience of one (United States) group and ignored not only reports
prepared by European Member States (UK and The Netherlands) but also extensive
studies by European nutrition experts.
In addition to work which was not
reviewed for the 1990 report, there is a large body of new evidence since 1990
(at least 177 published scientific studies on over 26,000 people) and 10 years
of further extensive use in many countries. Most of this new information comes
from conditions of free sale and is well documented.
In earlier reports it was suggested that
studies of the safety of VLCD should be undertaken under conditions of use in
the community. This information is now available from various studies and shows
the considerable levels of safety of the modern nutritionally complete very low
calorie (energy) diets.
During the SCOOP Committee meetings it
was accepted that though the term very low energy diet is scientifically more
accurate, the term very low calorie diet (VLCD) is so widely known and used that
this is the term that should be adopted for the SCOOP Task 76.3 Report. In
consequence we have also adopted this terminology.
Summary
This report reviews over
400 published scientific and clinical studies to early 2000, undertaken on
VLCDs, on over 50,000 people. Thus it is likely that VLCDs are the most widely
studied of all weight reducing diets. In addition, it records the main findings
in a series of audit studies undertaken during the routine use of VLCD.
The vast majority of the
studies identify the compositional standards and the length of administration
and this document concentrates on those papers. In almost 20,000 people use was
for more than four weeks, giving good evidence on safety of long-term use.
In addition current formula VLCDs have been used by well
over 25 million people in the international community over a period of over
twenty years.
In addition to
this critical review of the available safety and efficacy data in clinical use,
there have been a substantial number of recent experimental studies which have
shown that some of the earlier research reached erroneous conclusions. This
report reviews this data and highlights some important new scientific
conclusions which have practical implications.
Overall conclusions
A modern nutrient-complete VLCD provides
a highly effective and safe method of weight reduction. The use of VLCD has
benefits on excess weight related disorders which appear to be superior to those
of LCD or food based plans probably on the basis of the more rapid weight
loss.
On the basis of monitored clinical
experience coupled with recent body composition studies a scientifically based
standard for composition and labelling can and should be established for
VLCD.
In view of the
undisputed need to help the very large number who need to lose weight, as many
safe methods as possible should be made easily and readily available. This
includes VLCDs, where the safety can be shown to be at least as good as diets in
the >800kcal energy range. VLCDs should therefore be available on free sale
on the same terms as diets of over 800kcals (see Commission Directive
93/5/EC).
The following more detailed summaries and conclusions were
presented to the SCOOP Working Group:
Section
I Overweight and
obesity are rapidly and substantially increasing problems in all European Union
Member States (Section 1).
Over the past decade the prevalence of excess weight has increased by
some 50%. About 20% of the European middle aged are now obese and a further 30%
or more are overweight (Section 1.1) Excess weightis now accepted as having
reached epidemic proportions
Morbidity
increases steadily from a BMI of about 24 (towards the upper range of normal)
upwards. The problems associated with excess weight include not only serious
diseases, but also psychological and social ills (Section 1.2)
Excess weight is strongly
correlated with increasing mortality, so that at a BMI of 40 there is a greater
threat to life than smoking 20 cigarettes per day (Section
1.3)
The economic cost of excess
weight is substantial, with direct costs amounting to 1-5% of the health care
costs in most first-world countries (Section 1.4)
The evidence supports the view that all
effective and safe weight control methods should be readily available for
all those who have excess weight.
Section
II
The experimental studies and clinical experience reviewed here demonstrate that
products with an adequate and specified macronutrient and micronutrient
composition but an energy content below 800kcals per day (VLCD) are at least as
safe as those of higher energy content (LCD)
Special closely monitored clinical
studies in over 50,000 people, many for prolonged periods with laboratory
investigations and electrocardiographic monitoring show no evidence of
pathological changes as a result of the use of VLCD. This confirms the practical
experience of use of VLCD in over 25 million people during more than 20 years.
(Sections 2.1& 2.3)
The studies reviewed here show that
products with an adequate macronutrient and micronutrient composition, but an
energy content in the range 400-800kcals per day (VLCD) are at least as safe as
those of higher energy content LCDs at starting BMI levels down to 25 and
finishing BMI levels in the normal range (20 to 25). (Sections 2.3 &
2.4)
The submission about safety is based upon
the following data
:
Summary of the available
published data on diets under 800kcals
|
|
No
studies
|
%
|
|
No
subjects
|
%
|
|
|
|
|
|
|
|
|
Total
|
|
461
|
|
|
52,783
|
|
|
|
|
|
|
|
|
|
Date of publ
|
|
|
|
|
|
|
|
Up to
1975
|
9
|
|
|
340
|
|
|
1976-1980
|
25
|
|
|
1,525
|
|
|
1981-1985
|
72
|
|
|
2,591
|
|
|
1986-1990
|
121
|
|
|
8,096
|
|
|
1991-1995
|
139
|
|
|
23,887
|
|
|
After
1995
|
85
|
|
|
15,694
|
|
|
|
|
|
|
|
|
|
Energy cont
|
Per
day
|
|
|
|
|
|
|
Up to 450
kcal
|
280
|
66
|
|
31,949
|
66
|
|
Over 450
kcal
|
146
|
34
|
|
16,566
|
34
|
|
|
|
|
|
|
|
|
Protein
|
Per
day
|
|
|
|
|
|
|
Up to
50g
|
180
|
44
|
|
19,212
|
38
|
|
Over
45g
|
233
|
56
|
|
31,303
|
62
|
|
|
|
|
|
|
|
|
Carbohyd
|
Per
day
|
|
|
|
|
|
|
Up to
45g
|
292
|
73
|
|
40,608
|
90
|
|
45 to
50g
|
25
|
6
|
|
763
|
2
|
|
|
Over
50g
|
82
|
21
|
|
3,627
|
8
|
|
Use
length
|
|
|
|
|
|
|
|
Under 4
wks
|
81
|
18
|
|
17,006
|
33
|
|
4 wks or
more
|
371
|
82
|
|
34,705
|
67
|
Energy/day
|
<400kcal
|
111
|
27.4
|
4,182
|
9.1
|
|
400-599kcal
|
261
|
64.4
|
40,674
|
88.6
|
|
600-799kcal
|
33
|
8.1
|
1,053
|
2.3
|
Carboh/day
|
30-40g
|
149
|
44.2
|
34,194
|
80.4
|
|
41-45g
|
81
|
24.0
|
3922
|
9.2
|
|
46-50g
|
25
|
7.3
|
763
|
1.8
|
|
>50g
|
82
|
24.3
|
3,627
|
8.5
|
NB. The figures do
not total because some papers do not contain full information.
Several papers covering at least 500 subjects have been omitted because the full
paper could not be examined.
A
full listing of these studies is given as Appendix I and a full bibliography
for them is given as Appendix II.
Despite the fact that no deaths with
liquid protein diets (PLD) have been identified since 1977/1978, it is still
being suggested that experience with these diets have relevance. The information
relating to LPD was re-examined and confirmation given to the Working Group that
these have no relevance to current VLCD. (Section 2.3.1 &2.2)
Clinical studies have demonstrated
that:
i)There are a negligible number of
significant adverse reactions in the studies (over 50,000 dieters) or in routine
use in several millions under free sale use (Section 2.3)
iii) There is no damage to the
heart or other organs (Section 2.)
iv) Various other concerns
expressed in the previous reports on VLCDs (consequences of rate of weight loss,
additional difficulty in weight maintenance and weight cycling) are no greater
than with LCD (Section 2.5 & 2.6)
v) The results with VLCD are as good,
if not better than with the use of other methods of dieting (Section 2.6) In a
group study in which there is good compliance, the rate of weight loss depends
upon the energy level of the diet (Section 2.6).
vi) The only way to achieve
long-term weight maintenance is by a fundamental change in lifestyle. However
the results achieved by such change after weight reduction by VLCD are at least
as good as with those other non-invasive methods (Section 2.7)
vii) Cholelithiasis is not a specific
disorder of VLCD use and different formulations affect the incidence (Section
2.7). There is a requirement for essential fatty acids. If the essential fatty
acids are derived from normal fat (which would require above 7g per day normal
fats) this also provides sufficient fat to avoid cholelithiasis
Modern, nutritionally complete VLCDs are
not only more effective than all other non-invasive methods of weight reduction
but are at least as safe
Section III Many recent studies have been
undertaken which have established a clear understanding of the properties of
VLCD
1)A thorough examination of body
composition estimation has indicated that there is substantial lack of
reliability and reproducibility in most of the methods that have been used for
weight loss studies. With the exception of neutron activation, which is
expensive and not widely available, all the methods are indirect estimates. This
implies that the estimate is influenced by variation in formulae which are used
for converting the observation to the estimate (Section 3.1).
ii) Apart from technical errors in
the estimation, attention is directed to physiological variations that can
profoundly alter the results. Considerable attention to detail in the study is
necessary (Section 3.1.5)
iii) In consequence it is
inappropriate to compare in the same chart, data derived by different techniques
(Section 3.2.1).
iv) The most widely used reasonably
reliable indirect technique is hydrodensitometry and unless otherwise stated we
have concentrated on data derived by this technique.(Section 3.1.5)
v) Unrecognised analytical variation may
explain the conclusions of Forbes on compositional changes during weight loss
(Section 3.2.1)
vi)..The Keys (1950) Minnesota study has
been quoted as confirming that fat free mass (FFM) loss is greater in
individuals with less fat, who diet by any means. Re-examination of the data
indicates that while this may be true in those at BMI levels less than 20, at
these levels dieting is in any case un-necessary and contraindicated. It is
irrelevant down to the least level (about BMI 25) at which dieting is justified.
(Section 3.3)
vii) The loss of lean body mass
(protein) is inherent to any weight loss, regardless of energy intake, because
weight gained is not 100% fat. There is no proportionately greater lean body
mass loss with VLCD providing over 40g high quality protein per day than with
LCD (Section 3.4 & 3.5)
viii) Re-examination of the old data and
further new observations support the view peoposed by Garrow and others in the
1970s, that at all pre-dieting BMI levels between about 60 and 25, FFM
represents about 25% of the weight loss (range about 20-30% probably depending
on genetic factors). This is true for any energy value diets containing
appropriate macronutrient levels (Section 3.5)
ix)
Attention is directed to the
fact that as loss of lean body mass is inherent in any weight loss, there is an
obligatory nitrogen loss during weight loss. Hence excess nitrogen loss is only
relevant if it is greater than the obligatory loss. At daily intake levels of
40-50g protein in the diet, loss in excess of that which is obligatory is
unusual. (Section 3.7)
x)
There is no clinical or
valid experimental evidence which indicates that carbohydrate levels above those
currently available and widely studied, i.e. about 40-45g per day (about 90% of
the available clinical data) have any merits.(Section 3.8)
Compositional
standards.
From examination of the extensive
scientific work available (Appendices II & III), and consideration of the
various national and international regulations and codes of practice, the
compositional conclusions currently in force for VLCD
are:
Protein
Range of minima between 40-50g with a
minimum nutritional quality as defined by WHO/FAO (FAO, 1991)
Carbohydrate
Either no recommendation; or in some
regulations a range of minima for available carbohydrate between
40-50g.
Fat
A minimum of 7g neutral fat per day which
would provide not less than 3g linoleic acid and 0.5g linolenic acid with a
linoleic/linolenic acid ratio between 5 and 15
Micronutrients
This has been the subject of separate
consideration and these internationally agreed levels should be
adopted.
Fibre
The fibre recommendation should allow for
soluble fibres to be used. The minimum should be 10g per day. The available
carbohydrate component of this should be included in the carbohydrate
figure.
Energy
There
is a range of minima between 400-450kcal. The energy value per se has no direct relevance and the
minimum should be established based upon the energy provided by the defined
minimum for the macronutrient recommendations.
Having re-examined the clinical and experimental evidence which we have
submitted to the Working Group, we see no scientific reason for changing any of
the above views about the compositional standards which we submitted in March
2000.
Section
IV There is substantial medical and
scientific justification for modern nutrient complete formula diets with an
energy value less than 800kcals per day :
i) It is
widely accepted by scientists that formula diets are more effective than normal
food based diets for compliance in weight reduction (Section 4)
ii) There is no perfect single
weight reducing method and a variety of safe diets is desirable to suit
differing desires and prejudices. VLCD can have a significant effect on
motivation and compliance in some people. (Section 4)
iii) There is recent convincing
evidence that the rapidity of weight loss confers additional positive health
benefits independent of the weight loss in, for example, non-insulin dependent
diabetes mellitus and hypertension (Section 4)
Modern nutrient-complete formula VLCD
have an important place in weight reduction
Section
V The precautions for VLCD use
should be those which apply to any method for losing weight
i). The report endorses physiological
and medical contraindications and precautions that have already been extensively
published, but emphasises that these apply to all forms of effective weight
reduction and not just to VLCD (Section 4.1).
ii).As with any weight loss diet, medical
supervision is only necessary if there are medical complications (Section
4.2)
iii).Those with defined medical conditions,
those dieting for prolonged periods and those receiving prescription drugs
should seek medical advice and/or supervision – following the same advice as
those using LCD.
iv) .Continuous use of VLCD to the desired
weight is preferable to intermittent dieting for both physiological and
psychological reasons, and has no disadvantages (Section 4.3)
This report
supports:
·
The need for any product claiming weight
loss to demonstrate safety and efficacy.
·
Minimum compositional standards for all
diets, including those in official reports, and in the media.
·
Advice that those dieting for more than
three weeks by any method should seek medical advice.
SECTION I: OVERWEIGHT & OBESITY – THE NEED FOR
EFFECTIVE SLIMMING PLANS AND PRODUCTS
1.1
The
prevalence of excess weight
The increase in the incidence of obesity
is so great in most developed countries that it can be regarded as a pandemic.
Over the past decade obesity has almost doubled in many countries and the
average adult is currently adding an estimated one gram per day to its weight.
Since overweight (BM1 25 – 30) and obesity (BMI >30) are factors in both
mortality and morbidity, there is a real need not only to prevent any further
increase in the problem but also to reduce the weight of those who are already
affected.
There is no dispute that the ideal
approach to weight problems is to avoid them by a judicious change in the
lifestyle of the population. This involves an increase in physical activity and
a reduction in food intake, particularly foods high in fats. Such social change
has so far proved impossible to achieve. However, even if it can be achieved in
future, it will still be necessary to reduce the weight of the substantial
proportion of the population which is currently overweight or obese.
1.2 Excess weight
and morbidity
Numerous studies have shown that women
are far more likely than men to become overweight and that there is a higher
incidence of obesity in the lower social classes (both men and women) in most
industrially developed countries. Since the early 1980s there has been a
considerable increase in the prevalence of overweight and obesity in most
western countries. Thus, for example, Gregory et al. (1990); White et al. (1993)
and Cox (1993) all demonstrated that in the United Kingdom, the proportion of
those who were overweight rose by some 50% for women and 30% for men over the
decade of the 1980s. One of the recent British surveys (Central Statistical
Office, 1996), showed that the average weight for both men and women had risen
still further, such that the average BMI for each sex now lies in the overweight
range (average BMI men 26.0; women 25.8). Over the 15 year period from 1980 to
1995 the prevalence of obesity almost doubled (from 8% to 15% – Wilding, 1997).
At present, in the UK, 62% of adult women are either overweight or obese. And
the proportion is forecast to further increase (estimate 25% women and 20% men
obese early in the next millennium).
Nor is this confined to the UK. Recent
studies (e.g. Seidell, 1991; WHO, 1997) have found similar increases in many
countries. Thus in Europe some 15-20% of the middle-aged are obese (more in
Eastern Europe, less in Scandinavia).
1.3 Weight
increase and mortality
Excess weight is associated with a high
level of morbidity, embracing a wide range of disorders which both produce ill
health in the community and are a great burden on national health costs. These
include cardiovascular problems, diabetes, liver disorders and gall bladder
disease, some cancers, excess risk during surgery and a higher incidence of
accidents (Table 1.1). Added to this, increased weight increases the morbidity
in various chronic disorders (such as arthritis) and produces several serious
social and psychological problems.
Table 1.1 The increase in morbidity and mortality
associated with obesity (>30% overweight) in various medical
conditions
|
Disorder
|
Morbidity
|
Mortality
|
|
Diabetes
|
110-500
%
|
520-790
%
|
|
Cerebrovascular
accident
|
11-440
%
|
150-220
%
|
|
Coronary
heart disease
|
130-240
%
|
200-210
%
|
|
Cancer
|
|
130-160
%
|
|
Post-operative
wound infection
|
700%
|
|
|
|
|
It has been traditional to regard a BMI
between 25 and about 30 as a mild and largely cosmetic problem of negligible
health concern. This has been highlighted by the use of two different terms –
“overweight” and “morbid obesity” for
different excess weight ranges, though where the dividing line is placed differs
from one authority to another. The studies quoted above demonstrate that there
is a continuum of deteriorating health from about BMI 24. It must be concluded
that the arbitrary division into a morbid condition of obesity and a benign
condition of overweight is not only scientifically unjustified, but is a
dis-incentive to drawing attention to the need to consider any excess weight as
requiring action.
Thus all the information supports the
view that all effective and safe weight control methods should be readily
available for all those who are overweight
1.4Weight
increase and mortality
Over several years there have been many
studies which have examined the relationship between either the body mass index
or other indications of obesity and mortality. Among recent studies are those of
Garrow (1992), Pi-Sunyer (1993), Andres et al. (1993) and Manson et al. (1995).
Each has shown that as the weight increases so does the mortality. Garrow (1992)
has expressed it very vividly –“for example, a woman of height 1,58m would be in
the desirable range of weight for her height if she weighed 63kg. If she weighs
100kg [BMI 40] … the mortality ratio is about 250% of that at [her desired
weight]…so this degree of obesity is a greater threat to health than smoking 20
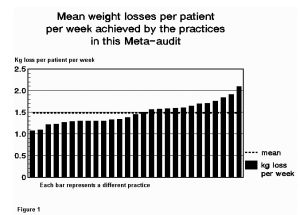
cigarettes a day.” (Figure 1)
However, while the relationship between
major weight increase and mortality is clear, the picture is a complicated one
if looked at in detail, because obesity is also associated with other disorders
which give rise to a reduced life expectancy. Other factors can also change
these related disorders and in consequence the relationship to weight is not
linear throughout the whole obese group. However, “the overall increase in
mortality is approximately 15% for every 10% that the person is above the normal
weight” (Marks, 1997). Reduction in weight produces a significant reduction in
the mortality risk. There is therefore every justification for those who are
overweight to attempt to reduce towards the normal level.

Figure 1.1
The relative risk of premature death compares with the level of
obesity/overweight (BMI). Based on Garrow (1981)
The relationship of weight and mortality
is also strongly correlated with the distribution of fat. Obesity with the main
increase of fat around the waist carries the highest risk, both for all cause
mortality and for that associated with cardiovascular diseases. Recent studies
(Cox & Whichelow, 1996; Ashwell et al., 1996) suggests that the ratio of
waist circumference/height is a very good predictor of mortality and that this
ratio is also a good predictor of reduction in risk when the weight is reduced.
There is evidence that it is more reliable than the BMI in this
respect
Recent studies (Iribarren et al.,1995;
Byers, 1995; Manson et al., 1995) have demonstrated that overweight per se (i.e.
any increase in weight beyond the normal) carries an increased risk and that it
is greater when the overweight is associated with other disorders.
Several of these studies have produced a
clear picture of an increase of serious and life shortening diseases from a BMI
of about 22 upwards. Typical charts for cardiovascular disease and cancer from
the paper by Manson et al. (1995) are shown in Figures 1.2a and 1.2b. A study in
a Finnish population (Rissanen, 1990) showed a highly significant (p =
<0.0001) linear rise in the weight range BMI 20 – 32.5 for coronary heart
disease and musculo-skeletal diseases, while in the United Kingdom Shaper et al.
(1997) reported that the risk of cardiovascular disease associated deaths, heart
attacks and diabetes all increased progressively from a BMI index of <20,
even after age, smoking, social class, alcohol consumption and physical activity
had all been adjusted for. Similar results have been reported by Manson et al.
(1987); Linsted et al. (1991); Lee et al. (1993) inter alia.
Indeed it is now apparent that the ideal
weight from the point of view of low mortality is about BMI 20 to 21. This
implies that it is not enough to concentrate on the treatment of the obese, but
that the management of those who are overweight, particularly when young, also
require attention quite apart from the fact that there is a steady progression
from overweight in youth to obesity in middle age
Figure 1.2 a) and b) Relative risk of death from
cardiovascular disease (a) and cancer (b) according to Body Mass Index amongst
women who never smoked (from Manson et
all, 1995)
|
Chi for trend =
8,84
P<0,001
(a) |
Chi for trend =
,96
P<0,001
(b) |
1.5The economic cost of obesity
Although studies in Northern Europe,
particularly Finland (Rissanen et al., 1990) had identified that there were
major direct economic costs associated with obesity, the first of the papers
which attempted to quantify the costs, emanated from the United States (Colditz,
1992). He considered the direct and indirect health costs involved based upon
1986 cost levels. He reached a figure of some $39.3 billion representing some
5.5% of the total health care costs in the United States (Table 1.2). His
figures only represented health care costs. The true economic costs would add
considerable sums to the overall cost to the community.
Table 1.2Estimated costs of five major disorders
associated with obesity
|
Total $ 39.3 billion
|
|
|
|
|
Non-insulin-dependent
diabetes mellitus
|
57
%
|
|
Gallbladder
|
30
%
|
|
Hypertension
|
20
%
|
|
Cardiovascular
|
19
%
|
|
Cancer
|
2.5
%
|
USA figures – 1986 (Colditz et al,
1992)
Subsequently, these economic costs have
been studied in Europe, the United States, Australia and New Zealand (Wolf &
Colditz, 1994; Segal et al., 1994; Seidell,1995; Levy et al., 1995; Seidell,
1997). The direct costs, i.e. those costs which are related to the diagnosis and
treatment of both obesity and diseases related to obesity amount to between 1 –
5% of the total national health expenditure in these countries. Seidell (1997)
specifically draws attention to the fact that these only represent the costs of
true obesity and to these should really be added those attributable to
overweight, which with the greater number of patients likely to be involved
would probably amount to at least the same level as those for obesity. To these
must be added indirect costs to society (sick pay, pensions etc); loss of
productivity from sick leave and early mortality; personal costs which arise
from higher insurance premiums, job discrimination, adaptations to cope with
disability etc. Thus the total costs, which have not yet been quantified, are
very large – placing a major strain on the economy of even the most industrially
developed country. These costs are likely to rise even more if safe and
effective diets are not made readily available.
SECTION II: THE
SAFETY OF VERY LOW CALORIE DIETS IN EXPERIMENTAL AND CLINICAL USE.
2.1 The Prime
Data
The literature on the management of
obesity in general and the use of VLCD in particular abounds in ex cathedra
statements unsupported by scientific data. To compound the misinformation
available in the literature, these ex-cathedra statements are then further
quoted as though they represented prime data, not only in other papers and
reviews, but also in national and international expert committee
reports.
The best way to
break this vicious circle is to examine and report the actual findings in true
prime data publications i.e. those that define the actual individual studies
with enough information to assess their significance. An attempt has been made
to identify and list for this discussion paper as much prime data as possible
for nutritionally complete formula diets with an energy value below 800
kcals.
This policy of
stressing the prime data also accords with the summary of the SCOOP 76.3 task
“Collection of data on products intended for use in very low calorie diets (EU
document C(2000)498)
It is accepted
that there are accidental “sins of omission and commission” within this
discussion paper, particularly caused by changes in formulations over the years,
but it is submitted that these do not significantly affect the
conclusions.
The data
comprises
2.1.1
Published monitored studies
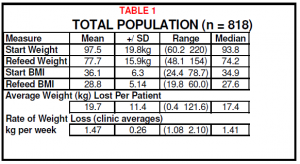
Special closely monitored studies in over
50,000 people who have received many different formulae all giving a daily
intake under 800 kcals. A substantial proportion of these represent
administration for prolonged periods and/or laboratory investigations and
electrocardiographic monitoring. A summary of this data is given in Table
2.1.
Table 2.1. Summary of the available published data on diets
under 800kcals
|
|
No
studies
|
%
|
|
No
subjects
|
%
|
|
|
|
|
|
|
|
|
Total
|
|
461
|
|
|
52,783
|
|
|
|
|
|
|
|
|
|
Date of publ
|
|
|
|
|
|
|
|
Up to
1975
|
9
|
|
|
340
|
|
|
1976-1980
|
25
|
|
|
1,525
|
|
|
1981-1985
|
72
|
|
|
2,591
|
|
|
1986-1990
|
121
|
|
|
8,096
|
|
|
1991-1995
|
139
|
|
|
23,887
|
|
|
After
1995
|
85
|
|
|
15,694
|
|
|
|
|
|
|
|
|
|
Energy cont
|
Per
day
|
|
|
|
|
|
|
Up to 450
kcal
|
280
|
66
|
|
31,949
|
66
|
|
Over 450
kcal
|
146
|
34
|
|
16,566
|
34
|
|
|
|
|
|
|
|
|
Protein
|
Per
day
|
|
|
|
|
|
|
Up to
50g
|
180
|
44
|
|
19,212
|
38
|
|
Over
45g
|
233
|
56
|
|
31,303
|
62
|
|
|
|
|
|
|
|
|
Carbohyd
|
Per
day
|
|
|
|
|
|
|
Up to
45g
|
292
|
73
|
|
40,608
|
90
|
|
45 to
50g
|
25
|
6
|
|
763
|
2
|
|
|
Over
50g
|
82
|
21
|
|
3,627
|
8
|
|
Use
length
|
|
|
|
|
|
|
|
Under 4
wks
|
81
|
18
|
|
17,006
|
33
|
|
4 wks or
more
|
371
|
82
|
|
34,705
|
67
|
NB. The figures in Table 1 do not always total
because some papers either do not contain full information or the information
indicates that a range of intakes used covers more than one category. Several
papers have been omitted either because the full paper could not be examined or
inadequate information is given on the content of the diet which was used. This
is particularly true of several recent papers which just use the designation
‘very-low-calorie diet’, without describing even the calorie content. There are
now several papers using a formula diet which provides 800kcal per day- So far
as possible these have also been omitted This has not been easy, because the
trade name of the diet is similar to that of an earlier version of lower energy
value and some papers do not clarify which formula has been used
A full listing of these studies is given
as Appendix I A full bibliography of them is given as Appendix II. This
bibliography also gives a list of additional papers examined over the period
1987 to 2000 during the preparation of the various versions of reports and
discussion papers on VLCD that have been prepared for different
committees.
2.1.2
Experience in general (mainly free sale) use
In addition to these published studies,
there has been extensive free sale use of modern very low calorie diets of
different formulations in many countries over a number of years.
This “free sale, predominantly not
medically supervised” use now covers substantially over 25 million people world
wide. It is submitted that the topic of dieting is so newsworthy in the general
media, that though this does not represent hard data on safety, such a level of
use with virtually no reported morbidity provides valid evidence that free sale
is entirely appropriate given adequate
labellng.
Despite extensive enquiry
concerning the regular media as well as the scientific literature, we have not
been able to find one single death which can validly be attributed to the use of
VLCD within this medically compromised group in the past 22 years, despite
extensive studies and free sale use by many millions of the population.
This can be contrasted with the extensive
literature which accumulated rapidly and dramatically in the late 1970s and
early 1980s during the brief period when “liquid protein diets” (which bear no
relationship to current nutrient complete diets) were available. Although these
tragic deaths associated with the use of liquid protein diets covered a period
of only about 12 months in 1977, with no further problems after they were
withdrawn from the market, they remain to this day a ‘spectre at the feast’. On
several occasions matters relating to them have been raised by the Working Group
and it is clearly important to put this spectre to rest.
2.2 Putting the
spectre of liquid protein diets to rest.
Doubt has been cast from time to time on
whether the daths in 1977 were indeed solely attributable to the use of liquid
protein diets or whether some of these subjects had been provided with slimming
diets of higher nutritional status. Accordingly at the request of the Working
Group, an examination was made of all the available evidence relating to these
liquid protein deaths in 1977 (Isner et al, 1979; the full report (dated 1979)
of the bureau of Foods, Food and Drug Administration committee meetings
(Contract FDA 223-75-2090), records of evidence submitted to the committee by
the Center for Disease Control, 1979; Food and Drug Administration, 1977,
Schucker & Gunn 1978, Sours et al, 1981; Federal Register, 1980; Federal
Register, 1982; van Itallie, 1984) Additional to this we have examined the three
papers which describe some of the original papers (Michiel et al, 1978; Singh et
al, 1978; Brown et al, 1978): the papers which describe other deaths during
therapeutic starvation for obesity (Cubberly et al, 1965; Kahan 1968; Spencer,
1968; Garnett, 1969) as well as the pioneer studies on PSMF in which there were
no recorded deaths. We have also examined the various AACE Positions
Statements on Obesity up to the 1998 revision in which, from time to time
comments appear on this problem. From this wealth of data and conjecture the
following information emerges:
·
Survival time was
related to the BMI.
–
Despite the fact that
there were over 200 commercial LPD in use in the 1976/1977 period in the USA
which were used by a very substantial number of dieters in the BMI range 25-30
there were no deaths in this group.
–
All the deaths occurred
in those over BMI 30.
–
There were more than 50
deaths attributed to LPD but only 17 of these were investigated. It is
acknowledged that the other deaths may have had a different pathology – the
situation of these is unknown.
–
Among the investigated
deaths the survival time is directly related to the BMI in the above 30
range.
–
The fact that those in
the 25-30 BMI range did not die is probably due to the relatively short use in
those at the lower weight, but it can not be held that “fat is
protective”.
–
In the above BMI 30
group it must be remembered that the total body protein before dieting was also
substantially above the normal. If one of the problems with the LPD was a
shortage of one or more essential amino acids, it follows that those with the
highest protein (hence amino acid) reserves would survive longest.
·
It is not true that
‘high quality VLCD’ were being used as a significant protein source.
–
No modern type VLCD
were available commercially in the USA until 1980.
–
Some PSMF type
non-commercial formulae of variable content were under study but the studies
which used these higher quality protein did not lead to any deaths, though it is
clear that the number of patients studies for over 2 months was so few that
deaths would not have been predicted on the basis of the estimate of the risk of
mortality from LPD (estimate some 1/700).
–
The dietary information
within the quoted LPD reports was, by its nature all hearsay from relatives and
friends and virtually none of it could be verified by independent
evidence.
–
There are several
references to the fact that “most consumed daily calorie intakes provided by 85
to 200ml… of hydrolysed collagen or gelatin estimated to supply approximately
300Kcal”. One of the original papers indicated that one patient took just 15ml
per day over the whole period.
–
The amino acid analyses
indicate that many of the tested products were virtually free of many of the
essential amino acids.
–
Three women “added high
quality protein to their” liquid protein diet. The amount is never stated but
examination of their rate of weight loss compared with the remaining patients
showed that the increase in calories must have been small. The conclusion of the
USA committee was that the exact cause could not be determined (inadequate
essential amino acids; ? electrolyte disturbances), that some supplementation
with casein may have undertaken by a few people, but this does not amount to
“use of high quality VLCD”.
–
There was only one man involved. The level of his use of the protein source (not a VLCD) other than LPD
is far from clear. One report suggests that he merely supplemented – “all had
used a LPMF diet as their sole source of calories for some months”, another says
“he used a protein product that was reportedly of high quality”. It is of
interest that this is the only autopsy that records “possible early
infarct”.
–
Starvation had
previously been shown to produce deaths of the type seen with LPD.
·
Deaths were not only
the result of self-medication without medical control
–
No less than 12 of the
17 patients whose deaths were examined were being treated by medical
practitioners. It is frequently suggested – inaccurately that all were
self-medicating.
–
A substantial
proportion were alleged to have had regular electrocardiograms while they were
receiving the LPD.
·
The deaths could not be
attributed to protein losses in the heart being greater than those in other
organs due to a more rapid protein turnover in that organ
–
The “weight of the
hearts….was decreased in proportion to the documented decrease in body
weight”.
–
There was no evidence
of increased loss of heart muscle protein as a result of the different heart
muscle turnover rate.
·
Removing liquid protein
diets from the USA market solved the problem
–
From the 1980 FDA
report and a further FDA report in 1982 it is clear that there were NO further
deaths attributable to weight reduction once the liquid protein diets were no
longer used despite the substantial free sale of a substantial number of
properly formulated VLCD most at that stage with an energy content in the range
300 to 400 kcal per day.
2.3 Clinical audits of
safety of VLCD
2.3.1 Specific audits
Nevertheless
from time to time it is suggested in official reports that “there has been a
lack of vigilance in gathering such information”. There is no evidence
whatsoever to support this contention. Indeed quite apart from vigilance by the
various companies monitoring adverse reactions reported in the medical and lay
media, there have been several extensive audits undertaken during use in the
community under health professional care. These include:
1.
An audit of 500 obese women
sequentially joining a modular (12 week) obesity management programme
(formulation: protein 43g; carbohydrate 38/45g) in the United Kingdom, of whom
85% completed 1 month and 50% completed 3 months or more. No serious untoward
events have been encountered during the ten years that the programme has been
running-
2.
Also in the United Kingdom,
a GP-based programme has been active since 1990. The data on the first four
years has been mislaid but it did not contain any significant adverse reactions.
Since 1993, some 31,000 patients have been treated and monitored by their own
practitioners following this programme (formulation for women: protein 43 g;
carbohydrate 38/45g: formulation for men: protein 57g; carbohydrate 33/60g). The
average duration of treatment was 16 weeks and the vast majority have been
followed for at least one year post diet. Many of the practices have submitted
audit results from these clinics to their respective health authorities. Twenty
five such audits were assembled in a paper presented at the Medical Research
Society in the UK and at the European Obesity meeting in Barcelona (Beeson
1994). Full medical records show that there have been no serious adverse effects
over the whole 10 years.
While these
audits cover the generality of the adverse effects during the use of VLCD there
is a possibility that they only represent studies in which the starting BMI was
well above the 30 level. Moreover it might represent those who did not reach the
lower level, which it has been suggested is particularly susceptible to adverse
effects.
As a result it
was decided to examine those papers in more detail in which it had been shown
that there was a significant component of subjects in which the starting BMI was
below 30.
2.3.2 Investigations of reputed deaths with nutrient complete
VLCD
·
Two papers by Wadden (JAMA:
January & June 1990) have been quoted frequently as information relating to
safety aspects of the use of VLCD, particularly at BMI levels between 25 and 30.
The following comments are relevant:
–
In the USA in the early
1980s a rumour, based upon an FDA Talk Paper, circulated that some six deaths
might have occurred using the Cambridge Plan International Diet. Emil
Corwin for the U.S. Food and Drug Administration on February 21st
1996 issued the following statement “no deaths have ever been attributed
to the use of the Cambridge Plan International Diet”… “during the last five
years, as many as 7 million persons have used Cambridge’s programs and products”
(Newsday, February 22 1986, page 2)
·
In 1989, Connolly, a general
practitioner in Ireland reported a sudden death which he alleged was the result
of the use of a VLCD. The heart muscle was examined by a British Home
Office pathologist who reported that there was no evidence of the pathology
associated with “liquid protein diets” and that there was no evidence that this
was a death that should be attributed to the use of VLCD
·
In 1993 Muller &
Grossklaus reported “Autopsy studies performed on 16 persons whose death was
considered to be related to the use of VLEDs showed that the weight of heart
decreased in proportion to the decrease in body weight” This report was taken to
represent recent deaths in Germany. In fact the reference he gives
is to Isner et al (1979) and this refers to the “liquid protein
diets”.
·
In various places in the
Wadden articles there is a statement about reduced safety at lower BMI levels.
The references are always the same – i.e. the work of Forbes and the repetition
of the Forbes views by others. I can not find any other evidence for the statements about
safety. The accuracy of the Forbes work is examined elsewhere in this discussion
paper (Section III)
–
In this respect, we would
draw attention to the recent paper by Professor Sir Colin Berry entitled
“Bellmanism: the distortion of reason” (Berry, 2000). The views expressed here
are very apposite and particularly on the “imperfect understanding and use of
science, in particular in the evaluation of data. Studies which have been
discredited are cited repeatedly… in relation to the precautionary
principle.”
2.3.3 Audits of subjects with BMI under 30
In some of the papers it is possible to
establish what proportion of the data represented experience at a BMI
under 30.
In order to make the necessary
calculations it would be necessary to have adequate information to determine
that not only is there good compliance on average within the cohort, but that
the compliance is equally good across the weight range.
It is abundantly clear from the text in
many of the clinical papers that a proportion of those studied have lost such
substantial amounts (or proportions of their starting weight) that they have not
only moved into the BMI <30 range (if they were not there at the start), but
have achieved the normal BMI range. This is obvious if it is appreciated that
the compliant VLCD dieter, loses on average between 1 and 2kg/week. For a woman
of average current height, one BMI unit is equivalent to some 2.64kg. The
published clinical papers indicate that on average over 80% of the dieters are
women. For the men one BMI unit weight equivalent is more but the rate of weight
loss is greater.
Thus with the average weight loss per
week with the majority of the current commercial VLCD, there is a BMI change at
the rate of between about one BMI unit each 2 weeks. For those who start at BMI
30, a BMI about 25 (i.e. down to the normal weight level) will be achieved in
about 8-10 weeks, at least three-quarters of which will be below BMI 30. At
start BMI 35 the average time to normality will be about 18 weeks, with about
half that period below BMI 30.
There are 3 papers which provide
enough information tobe able to calculate, with reasonable accuracy, the proportion of the VLCD
dieting period which represents a BMI level below 30. The basis of the
calculation is such that even for these three studies it is clear that it does
not represent hard data. Nevertheless much of the data cross checks and is
sufficiently representative to be useful, bearing in mind that there are no
serious side effects in the whole series. The information covers several
previously published smaller cohorts, but the three papers concerned are those
of Kirschner et al (1988); Kanders et al (1989) and Bode (1999).
These cover observations using VLCD at
300, 420 and 770kcal per day, though it is not possible to establish with
certainty the exact proportion at each intake because the formulation changed
over time. One merit of all these studies is that they represent data for
observations of at least 12 weeks VLCD dieting a long enough period for any
major adverse effect to occur.
The information from these studies is
summarised in Table 2.2.
Table 2.2 Data on the three papers from which
information on the safety of VLCD at lower BMI levels can be gauged.
|
Ref
|
Total
subjects
|
Starting
data (BMI)
|
VLCD
dieting
|
VLCD
weeks BMI < 30
|
|
|
Mean
|
S.D.
|
Lowest
|
Av
wks
|
Total
weeks
|
Av
BMI lost
|
Total
|
Proportion
|
|
Kirschner
et al ’88 – men
|
603
|
34.9
|
0.95
|
|
13.2
|
7,960
|
9.23
|
3,327
|
41.8%
|
|
– women
|
2,348
|
37.5
|
0.80
|
|
14.1
|
33,107
|
6.8
|
745
|
2.25%
|
|
Kanders
et al ’89 – men
|
143
|
38
|
|
|
16
|
2,288
|
7.6
|
?
|
<5%
|
|
Women
|
718
|
35
|
|
|
16
|
11,488
|
6.65
|
2,849
|
24.8%
|
|
Bode
1999
– men
|
2,142
|
40.3
|
23.2
|
23.2
|
14
|
29,988
|
10.1
|
2,527
|
8.4%
|
|
–
women
|
10,754
|
38.9
|
6.6
|
23.9
|
14
|
150,556
|
6.7
|
18,481
|
12.3%
|
* excluding those not
completing dieting phase
The important points to note
are
·
For those with a BMI above
35, dieting for at least 12 weeks is necessary before the BMI falls below
30
·
In a major proportion of the
USA literature, with a very high initial BMI level and a short period of VLCD
use there is relatively little data at BMI levels <30
·
On the other hand, in
Europe, VLCD have been used at lower starting BMI levels and, in consequence
there is greater evidence of safety in the range 25 to 30.
On the basis of
this evidence a reasonable proportion of the VLCD dieting for these studies was
at BMI < 30. Since these represented experience in a substantial number of
dieters for a period of at least 12 weeks, there is substantial evidence of use
of VLCD in the BMI range (i.e. 25 to 30) for which further information was
required
Taking each of
these papers (Kirschner et al 1988; Kanders et al 1989; and Bode 1999)in
turn:
·
Kirschner summarises
his experience thus: “Complications of obesity i.e. hypertension, type II
diabetes mellitus and hyperlipidemias were remarkably improved after weight
loss. Complications of the VLCD including cardiac abnormalities, were
minimal”
The relevant
portion of the paper reads:
“Complications. A list of side-effects
and complications is presented in Table 4.
Table
4. Complications observed in patients on supplemented fast.
Cases
1)
Acute
gout
8
2)
Foot drop
(temporary)
2
3)
Acute
psychosis
4
4)
Diabetic
ketoscidosis
2
5)
Late hair
loss
10%
6)
Cardiac arrhythmias
Supraventricular tachycardia
(hypoglycemia)
1
Multifocal
PVCs
2
The most common problems noted were early
postural lightheadedness and tiredness, The most common late complaint was that
of mild transient hair loss, occurring in approximately 10 percent of the
population. Other complications included eight cases of acute gout, two cases of
foot drop, (thought to be due to sciatic nerve compression from leg crossing
during or after weight loss), and four cases of acute psychosis occurring in
women and generally thought to be a form of sexual panic.
In
view of the great concern regarding cardiac arrhythmias in patients on VLCDs we
carefully screened for such occurrences. Over the 8-year period, we documented
only one patient who developed a supraventricular tachycardia clearly related to
hypoglycemia ans corrected with intravenous glucose supplementation. Two
patients required hospitalisation for the development of palpitations associated
with multifocal PVCs. To date, we have had no unexplained deaths in contrast to
the experience with liquid protein diets.
Non-complications. In view of the genuine
concern as to the overall safety of VLCDs there were several important
non-complications to record, including: (1) coronary pypass surgery without
complications in eight patients; (2) major breast surgery without complications
in 12 patients; (3) pregnancies occurring while patients were on VLCD (without
subsequent complications) in six women in whom the diet was subsequently
discontinued.”
To put this paper in context it should be
appreciated that this represented something in excess of 40,000 weeks dieting
experience in 4026 patients at 420kcal/day with some 10% in the BMI range
<30. The quoted paragraphs followed several that detailed the beneficial
effects of VLCD on medical problems in this same patient cohort.
·
The equivalent paper by
Kanders et al (1989) gives a substantial amount of information about beneficial
effects. The phrasing of the report suggests that side effects were not a
problem but there is no specific reference to side effects throughout the whole
paper. It is abundantly clear from the nature of the paper, that, had side
effects been a problem, they would have been recorded.
·
The same situation is true
of the report by Bode (1999). He describes reasons for the subjects stopping the
use of the VLCD but these are primarily social. There are no significant medical
problems.
·
We have also obtained access
to the detailed information relating to LipotrimÒ a monitored VLCD programme (Kreitzman
& Beeson, 1996). This provides an indication of the VLCD dieting pattern in
the practical commercial area and moreover gives some indication of the post
diet period, though not over a prolonged period.
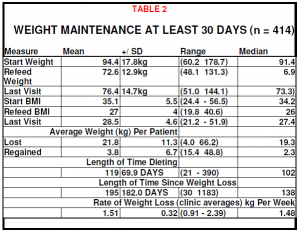
This study by Kreitzman & Beeson
(1996) was undertaken with trained independent medical observers. Again, no VLCD
related adversa effects were reported.
An audit of 746 case records was made.
This covers an overall period of total food replacement (TFR) by VLCD of 13,446
weeks; a total weight loss in the group of 15,657Kg representing an
average weight loss for each dieter of 20.99kg at an average of 1.2kg per
week.
Of the 746 dieters 140 started below BMI
30. The average BMI before dieting was 28.54 and that at the end of the TFR
period 24.06 (12.16kg) achieved on average in 78.84 days (11.2 weeks) at an
average of 1.08kg per week. All these spent their whole TFR at BMI <30
representing 1,568 weeks TRF. As a matter of interest the average follow up for
this group after re-feeding was 35 weeks and at that stage 79% had maintained
all their lost weight with the average regain under 0.9BMI unit.
The remaining 606 dieters started at
average BMI 34.6. They lost 23.03kg weight on average at an average of
1.18kg/week (total weight loss in this group 13,955kg). Their average number of
days on TFR was 137.10 days (19.6 weeks), achieving an average BMI at the end of
the TFR period of 26.08. Their total TFR period was 11,878 weeks of which 5,465
was under BMI 30.
This means that in this whole group, out
of 13,446 weeks VLCD use, no less than 7,033 weeks (something over 50%)
represented experience at BMI <30. In no dieter at any stage was there any
serious or worrying side effect.
2.3.4 Audits on the
prime data
It was also considered important to
examine the prime data in more detail to determine whether the information
provided covered the broad range of the energy and carbohydrate levels (rather
than just high carbohydrate levels providing energy levels close to
800kcals.
The results of this further analysis are
shown in Tables 2.3 a and b
Table 2.3 A further split of the original data into
Table a) <400kcal, 400-600kcal, 600-800kcal and b) carbohydrate levels
30-40g, 40-45g, 45-50g and >50g..
|
Kilocalorie content
|
Number of Studies
|
Number of subjects
|
|
<400
|
111
|
27.4%
|
4,182
|
9.1%
|
|
400-600
|
261
|
64.4%
|
40,674
|
88.6%
|
|
600-799
|
33
|
8.2%
|
1,053
|
2.3%
|
|
Carbohydrate content
|
Number of studies
|
Number of subjects
|
|
30-40g
|
149
|
44.2%
|
34,194
|
80.4%
|
|
41-45g
|
81
|
24.0%
|
3,922
|
9.2%
|
|
46-50g
|
25
|
7.4%
|
763
|
1.8%
|
|
>50g
|
82
|
24.3%
|
3,627
|
8.5%
|
It should be
noted that these figures differ slightly from those in Table 1 – some categories
were not represented and for some a more detailed analysis was not
feasible.
Nevertheless,
the further analysis demonstrates not only that a major proportion of the data
was derived from VLCD with an energy value less than 600kcals, but that over 90%
of the subjects were receiving a daily carbohydrate level below 50g.
2.4 Special tests for
safety
2.4.1.Laboratory
studies
Several of the published clinical studies
have investigated laboratory parameters of organ change (eg cardiac,
haemopoietic, hepatic, renal) on a regular basis. Many more have
undertaken spot laboratory checks. These have demonstrated evidence of
improved health due to the weight loss but no adverse effects from the use of
these diets.
2.4.2.
Electrocardiographic evidence of cardiac integrity
It was suggested in some of the earlier
reports that even if there appeared to be no overall excessive loss of protein
during the use of VLCD, there might be specific extra and dangerous protein loss
from the heart or other vital organs. However, as mentioned previously, clinical
observations and laboratory investigations over a period in excess of 20 years,
on more than 50,000 subjects using a very wide range of products of different
composition with an energy content under 800kcal, have not demonstrated that any
such problem exists. Nor is there any theoretical reason why damage to specific
organs should occur.
Specifically there is extensive
electrocardiographic evidence of cardiac integrity.
Obesity itself can produce cardiac
changes (Hinkle et al 1969; Eisenstein et al, 1982; Frank et al, 1986; Carella
et al 1996; Quaade et al 1996),). Indeed it has been calculated that an
obese cohort subjected to surgery has 40 times the risk of sudden death compared
to a normal weight cohort (Drenick & Fisler, 1988). Because the use of
the seriously nutritionally deficient liquid protein diets in the early 1970s
(which bear no relationship to the
modern VLCD) led to fatal cardiomyopathies (FDA 1979; Sours et al 1981; Isner
Sours et al 1981; Van Itallie et al 1984, random electrocardiographic recordings
and regular Holter monitoring have been an important feature of studies on the
modern very low energy diets in order to confirm that they do not have similar
adverse effects.
The 12 formal studies (summarised in
Table 2.4) all confirm that well formulated very low calorie
Table 2.4 Studies which examined the
electrocardiograph by Holter monitoring at intervals during the use of
VLCDs
|
Reference
|
Number
|
Duration
|
|
|
|
|
|
Fisler et al
1982
|
10
|
40-55
days
|
|
Amatruda et al
1983
|
6
|
40
days
|
|
Phinney et al
1983
|
10
|
28
days
|
|
Ms Lean Baird
1985
|
13
|
4
weeks
|
|
Drenick et al
1985
|
16
|
40
days
|
|
Lockwood et al
1985
|
11
|
40
days
|
|
Amatruda et al
1988
|
6
|
40
days
|
|
Kirscher et al
1988
|
4026
|
Various details of
monitoring unclear
|
|
Weigle et al
1989
|
11
|
95 days
average
|
|
Moyer et al
1989
|
24
|
6
weeks
|
|
Anderson
1990
|
104
|
8
weeks
|
|
Doherry et al
1991
|
12
|
16
weeks
|
diets produce no evidence of adverse
effects on cardiac function. Additionally Linet (1983) ans Singer (1981) found
no abnormality in food based diets (with added vitamins and minerals) at energy
levels below 600Kcals/day.
Indeed calculations demonstrate that the
incidence of sudden death in those being treated with VLCD well below the level
which would be predicted from their age and weight
Examination of
the “liquid protein diet” data on the 17 deaths that were studied (FDA 1979;
Sours et al 1981; Van Itallie et aI 1984) show that the shortest period to any
cardiac abnormality was several weeks. As Meuller and GrosskIaus wrote ( 1993)
:
“Electrocardiographic changes do not
become evident before 4-6 weeks of hypocaloric dieting” and “In subjects on
VLEDs electrocardiograms are usually negative up to 4-6 weeks” and “a well
supplemented VLED has fewer adverse effects on the electrical activity ofthe
heart” (In fact examination of the original data suggests that the figure is
more like 8 weeks than 4-6 weeks)
Hence the 12 ECG
studies quoted here are not as valuable as they would appear at first sight
because most cover the period before electrocardiographic changes wouId be
expected. It must however be stressed that since 1978 there is no confirmed
evidence of electrocardiographic changes at any stage.
This raises the whole question of the
suggestion made by some authorities that regular routine electrocardiographic
examination should be undertaken (even as frequently as weekly) on all those
using VLCD. This suggestion has no validity-.-.
·
The data indicates that the
only reliable method for determining changes is by Holter continuous monitoring
which is clearly impracticable. Thus in a study by Lantigua et al (1980) 3 out
of the 6 subjects deliberately subjected to a hydrolysed collagen diet with
added tryptophan showed cardiac conduction abnormalities, of which none were
detected by 12-1ead ECG, only by continuous Holter monitoring.
·
In six of the 17 who died in
the liquid protein tragedy, normal ECGs had been found while they were taking
the liquid protein diet.
·
There is no agreement about
the predictive relevance of any electrocardiographic features that might be
found.
One recent
widely publicised study (Greenway et al 1994) purports to demonstrate changes
(particularly in the Q-T segment) related to the energy rather than the protein
content but the changes reported are those seen commonly in untreated obese
people and have no significance relative to the safety of VLCD (Quaade, 1996).
Moreover Hinkle et al ( 1969) pointed out that ” disturbance of heart rhythm and
conduction occur in apparently healthy people with high frequency” while in the
study by Carella et al ( 1996) between 41% and 53% (depending upon the method of
determination) of obese people showed a prolongation of the Q-T interval before
any dietary intervention.
It has also been
postulated that since the protein turnover of myocardial proteins differs from
that in skeletal muscle, this may produce a failure of protein conserving
mechanisms in the heart and greater risks to that organ. Mueller &
Grossklaus (1993) have pointed out that there is no failure of
protein-conserving mechanisms in the heart for ” the weight of the heart
decreased in proportion to the decrease in body weight” and “Myocardial
wasting…is not necessarily associated with reduced functional capacity” and “A
24-week of semi-starvation resulted in a weight loss of 15-20kg…but not
circulatory insufficiency or heart failure” and “These data suggest a normal
myocardial fiber performance in response to semi-starvation”. These views
expressed by Mueller & Grossklaus are in accord with the earlier
observations of Smith (1928) and Amad et al (1965) that the weight loss in the
heart during starvation is proportional to that lost in the rest of the body
.
The relationship between heart weight and
body weight also applied to those who died in the 1977 liquid protein diet
tragedy (Sours et al 1981, Isner, Sours et al 1981 and Van Itallie et al 1984)
while none of these 17 dieters showed untoward evidence of heart muscle
insufficiency.
2.5 Data
on side effects
2.5.1 General side effects
A relatively
small proportion of those taking VLCD experience side effects. The risk of side
effects is greater if the dieter does not follow the directions given on the
diet pack or by any adviser (particularly of strict compliance to the diet and
to drink substantial quantities of water while taking the VLCD). The vast
majority of these side effects are minor and easily corrected. They occur at two
distinct phases – either within the first few days of starting the diet or after
several weeks of VLCD use. The main early side effects are shown in Table
2.5
Table 2.5 Early side-effects, possible mechanisms
and appropriate actions

The minor and non-dangerous nature of
these side effects is clear. Perhaps the only one which might require some
further attention is gout, but throughout the whole period during which one of
us (JM) was advising VLCD to dieters during the early trials, He did not
encounter a single episode of gout. We have also discussed this with others with
extensive VLCD experience who confirm that in practice they have never seen a
case of VLCD generated gout.
It is clear that
the major cause of the early side effects is that the advice about the need for
strict diet compliance and a high fluid intake during the use of VLCD have not
being followed.
A list of the main later side effects is
given in Table 2.6 All these side effects may be found with any successful
weight loss process, including surgery. Reassurance is normally all that is
required.
Table 2.6 The main side effects encountered after
prolonged use of VLCD.

2.5.2 Cholelithiasis
For well over 50
years it has been known that there is an increased incidence of cholelithiasis,
particularly cholesterol stones, with obesity (Gross, 1929) and this has been
confirmed by many recent epidemiological studies- These demonstrate that the
incidence of gall bladder disease in the morbidly obese varies from 28% to as
high as 45%, while over 80% show histological abnormalities in the gall bladder
(Williams et aI., 1977; AmaraI & Thompson, 1985; Maclure et al, 1989;
Bennion & Grundy, 1975; Bennion & Grundy, 1978; Tudevant et al, 1973;
Kucio et al, 1988. Everhart, 1993; Sichieri et al, 1991; Thijs et al, 1992; inter alia)
It is also
known that changes in food intake in the normal or obese, by whatever means
(total parenteral nutrition (Roslyn et al. 1983; Messing et al 1983), isocaloric
cholesterol lowering diets, traditional weight reducing diets (Everhart 1993),
jejuno-ileal bypass, gastroplasty (Shiffman et al 1993), VLCD) resuIt in an
increase of cholelithiasis. Moreover other factors, which have no relationship
to weight loss can also cause an increase in gallstone formation in the obese
These include multiple parity (Grodstein et al, 1994, though this is disputed by
Maclure et al 1989), high energy intake (Maclure et al, 1989), cigarette smoking
(Grodstein et al 1994), and current and long-term use of oral contraceptives
(Grodstein et al,1994)- In contra-distinction to these a moderate alcohol intake
as opposed to abstinence is reputed to reduce the gallstone incidence in the
risk population (Maclure et al 1989; Grodstein et al 1994).
Thus there are
many confounding factors which may play a role in any studies of the effects of
diet on the genesis of gallstones. The picture has been further confused by the
fact that many of the recent studies compare modem ultrasound measurements
during VLCD dieting or surgical intervention with previous studies based
entirely on clinical examination incidence. The extent of the difference between
the symptomatic and ultrasonographic incidence is clear from the Shiffman et al,
(1993) study. Following bariatric surgery in 230 patients, he found an incidence
of gaIlstones of 37% by ultrasonography aIthough only 10% showed any
symptoms.
It has been suggested, particularly in
the 1980s and the first half of the 1990s that a rapid loss of weight, such as
that produced by the use of VLCD or following jejuno-ileal bypass and
gastroplasty leads to a higher incidence of gallstones than that which results
from a slower loss of weight (e.g. that which results from a 1200kcal diet). A
careful examination of recent studies of the reputed lithogenic effect of VLCD
shows no clear evidence that this method of weight reduction leads to any
greater incidence of gallstones than other methods which produce the same
overall weight loss (Sturdevant et al, 1973; Mok et al, 1979; Schlierfet al,
1981; Wattchow et al, 1983; Messing et al, 1983; Roslyn et al, 1983; Anderson et
al., 1984; Amaral & Thompson, 1985; Bolondi et al., 1985; Broomfield et al
1988; Jacob et al., 1989; Janowitz et aI., 1989; Liddle et aI., 1989. Yang et
aI, 1990; Marks et al., 1991; Little & Avramovic, 1991; Shiffman,1991; Hoy
et al., 1991; Mazzella et al., 1991; Shiffman et al., 1992; Karnrath et al.,
1992; Heshka et al; 1992; Yang et al, 1992; Dammbach et al, 1993; Everhart,
1993; De Filippo et al., 1993; Festi et al 1993; Spirt et aI 1995; Gebhard et al
1996).
Examination of
the literature shows that, with very rare exceptions, claims of increased
incidence of cholelithiasis with rapid weight loss are American. The European
literature is devoid of such reports and conversations with those European
experts who have used VLCD extensively confirm that gallstone formation has not
been a problem. Perhaps even more importantly, in those papers in which the
details of the weight loss programme are recorded, the majority stem from two
commercial weight loss products widely used in the USA but not in
Europe.
If instead of
just taking the total energy intake, one examines the energy sources involved,
the picture becomes more clear (Table 2.7). Unfortunately no formal study has
been undertaken with the equivalent of the typical European diets (under
600kcals with about 7g fat per day) although there is substantial evidence from
adverse effect incidence in large scale studies in Europe- One of the best
studies is that of Festi et aI, 1998. They compared two VLCD with very similar
energy content but 9glday difference in the fat content. The number of patients
in each group was small, but there was a significant difference (p= <0.01) in
the incidence of new gallstones.
Table 2.7 Relationship of fat intake per day to
percentage of cholelithiasis.

Probably due to
the number of confounding factors, the relationship between the fat intake and
the gallstone incidence is not quite uniform, but there is a very strong
indication that it is the level of fat in the diet rather than the calorie level
per se, which is of prime importance. The mechanism involved would appear to be
the extent of biliary wall motility and regular gall bladder emptying (Kucio et
al, 1988; Marks et al, 1991; Mazzella et al, 1991; Festi et al 1992; Shiffman et
al 1995; Marks et al 1996)-
The available
data, particularly the fact that cholelithiasis is virtually unknown as a
complication with the widespread use of European commercial VLCD, suggests that
a daily intake of about 7g fat is necessary to ensure that gallbladder
contraction is normal. This fits in well with the observation that United States
diet programmes are associated with a higher incidence of gallstones than
European. It also explains why, when one United States commercial formula was
changed, with the addition of extra fat per day, the incidence of reports of
gallstone problems recorded in the American literature almost ceased.
It is clear from
all the evidence that any effective weight reduction leads to an increase in
cholelithiasis during the weight loss. Subsequently the risk is less.
Formulation differences and advice on fluid intake appear to be important.
Whether high protein levels encourage cholelithiasis (by reducing gall bladder
contractions) is not clear. However higher fat levels do discourage gallstones
(by increasing regular gallbladder contractions). As already noted, the
recommended fat level in VLCD (to provide essential fatty acids) of about 7g per
day is advantageous from the point of view of reducing the incidence of
gallstones.
2.5.3 Bone density
During the past few years it has
been suggested that the use of VLCD for weight reduction might lead to calcium
deprivation similar to that reputed to occur during the use of a high fibre
weight reducing diet (Avenell et al, 1994)
In consequence,
several studies have been undertaken to determine the factors causing loss of
bone density in post-menopausal women and whether prolonged use of VLCD (up to
15 weeks of continuous use) would lead to a similar loss of bone mass to that
reputed to be seen with high fibre diets.
For example Van
Loan et al (1998), using dual energy X-ray absorptiometry studied fourteen women
during a 15 week diet period, over which period they lost weight at an average
of 1 kg per week- They found no loss of bone mineraI caIcium in spite of the
marked loss in weight although there was a small loss of bone density. This was
equivalent to the findings of Compston et al ( 1992) during an 8 week study with
a VLCD.
From other
recent studies (Pritchard et al, 1996; Brot et al, 1997, Ensrud et al, 1997,
Willing et al, 1997) it is clear that, as could be logically expected, there is
a direct relationship between bone density and body weight. It is largely the
strains on the bones that determines their density. Whether weight is lost
intentionally (by whatever means) or unintentionally, the bone density is
reduced roughly in proportion to the loss of weight..
2.5.4 Data on eating
disorders.
It has also been suggested that VLCD may
be abused leading to eating disorders such as anorexia and bulimia. There is not
one iota of evidence for this. These disorders are entirely psychological in
origin. By the very nature of these disorders, which are concerned with false
body image, it would be anticipated that there would be an association with
various forms of dieting. However because there is an association, this in no
way implies that dieting is causative.
Even if they were not psychological,
those patients who are involved try to avoid VLCD because they are too energy
dense- They choose less energy dense methods of reducing their weight since the
volume of the alternative low energy dense diets reduces the patient’s hunger
with less energy intake.
2.6 Data
on aspects of use and control in practice
2.6.1 VLCD and the resting metabolic rate reduction during and
after dieting
Several recent
studies (Apfelbaum, 1993. Van Gaal et al., 1992; Coxon et al., 1992;
Kreitzman, Johnson & Ryde,
1992; Rattan et al., 1989) have demonstrated that the initial 15% reduction in
resting metabolic rate is a physiological response to reduced food intake within
the first few days of dieting and is not related directly to the actual energy
intake or to the amount of weight loss. The subsequent long term reduction in
the resting metabolic rate depends on the extent of the weight loss irrespective
of the method and energy levels by which it is achieved (Figure 2.1) (James et
al, 1978; Rattan et al., 1989. Van Gaal et al, 1992; Wadden et al., 1992; Coxon
et al., 1992; Wadden et al., 1990; Kreitzman, Coxon et al., 1992; Kreitzman,
Johnson & Ryde, 1993).
Figure 2.1. The effect of excess body weight on
resting metabolic rate (RMR). Based upon James et al (1978)

It is now clear that the formulae
developed by Schofield et aI. (1985) linking the resting metabolic rate to the
weight are correct and that the views of the Wadden group, heavily quoted in the
1990 SCF Report that the fall in metabolic rate depended upon the rate at which
the weight was lost during dieting were at error
2.6.2 The relationship
between energy deficit and rate of weight loss.
The study by
Kreitzman et al. (1993) demonstrated that the total daily energy expenditure is
not influenced during dieting, whatever the energy intake. The weight loss
showed a high correlation with the total energy expenditure (r = 0.82). In
consequence, in those studies where special attention was directed to ensuring
compliance, the rate of weight loss per week, which depends on the energy
deficit shows good correlation with the energy intake, after the first week of
dieting, during which glycogen and the attendant fluid loss complicate the
picture (Table 2.8)
Table 2.8 Average weight loss per week with
various weight loss procedures
|
Weight
loss procedure
|
Average
loss/week women
|
Reference
|
|
Exercise
alone
|
0.1
kg/week
|
Garrow
& Summerbell, 1995
|
|
1200kcal
diet daily
|
0.3-0.5
kg/week
|
Heshka et
al, 1996; Wadden, 1993; Topubro & Astrup,
1997
|
|
800kcal
diet daily
|
0.5-0.7
kg/week
|
Garrow,
1993
|
|
300-500kcal diet
daily
|
1.0-1.5
kg/week
|
Pekkarinen
et al, 1996 Tyttig & Rossner, 1995 Hoie & Bruesgaard, 1995, Rude
et al, 1993; Wadden, 1993; Toubro & Astrup,
1997
|
These figures represent averages over at
least an eight week period. Similar conclusions were drawn by Jensen &
Quaade (1996) using somewhat different criteria- It must be noted that, though
the correlation is good for groups of dieters, examination of the individual
weight loss does not always show such a good correlation even when compliance
appears to be good. There are various possible explanations for this (Marks
& Howard,1997).
As would be anticipated from what has
been said about the resting metabolic rate being dependent on the body
mass and not on the rate of its change during dieting, clinical experience and
experimental studies show conclusively that there is no greater difficulty
maintaining the target rate after rapid than after slow weight loss. The
question of weight maintenance is dealt with later.
2.6.3 Weight
cycling
Weight cycling
(yo-yo dieting) does not lead to increased fat stores, reduced metabolic rate,
and less effective weight loss with each cycle as was previously suggested. In
several excellent studies (Forbes, 1987; Steen et al., 1988, Prentice et al.,
1992; van Dale & Saris, 1989; Kamrath et al, 1992; Wadden et al., 1992;
Beeson et al., 1989; Bene et al., 1991; Blackburn et al., 1989; Brownell, 1989.
Chen & Cunnane, 1993; Goldberg et al., 1990; Jebb et al., 1991; Kamrath et
al., 1990; Kaplan et al., 1992, van der Kooy et al 1993) it has been shown that
weight cycling does not have an adverse effect on body composition. Hence the
metabolic rate and rate of weight loss of the various cycles are
equivalent.
Earlier studies
in Sweden and the USA (Lissner et al, 1988 a&b; Lissner et al. 1989)
suggested that weight cycling increases coronary disease and hypertension risk,
but this was not confirmed in more recent studies undertaken by the group who
made the original observation (Lissner et al. 1990, 1991; Brownell & Rodin,
1994). It is important to appreciate that Castelli, one of those involved in the
Framingham Heart Study, subsequently affirmed that there is no evidence of any
undesirable physical sequelae from weight cycling. This has been confirmed by
further more recent studies (Willett et al 1995, Wing et al 1995, Itoh et al
1996, Field et al 1999). Nor could Bartlett et al. (1996) find any untoward
psychosocial sequelae.
There had also
been some papers which suggested that weight cycling produced unstable body
weights which in turn lead to a greater mortality risk. More recent studies have
confirmed that there is no relationship between weight cycling and risk of
premature mortality and that the previous observations resulted from a
confounding effect of weight loss due to disease (Williamson 1996, French et al
1999).
But even if such an adverse effect exists,
weight cycling is found with all forms of dieting and no causative relationship
between VLCD and the reputed increased risk has been established. Hence it has
no relevance to the current considerations though it has been regarded in the
past as a problem alleged to be related to VLCD.
2.6.4 Continuous versus intermittent use
Some reports state that when a
considerable weight loss is necessary, this should be done in a series of three,
four or six week periods separated by one week or more when the diet is
supplemented by ‘normal’ food of a higher calorie level.
There is no
scientific reason for this procedure, indeed from the point of view of
experience it is highly undesirable and de-motivating. The main effect of the
higher calorie periods is to increase weight by the accumulation of glycogen and
water which serves no useful purpose. Indeed, some studies can be interpreted as
demonstrating that intermittent dieting in this fashion may lead to increased
protein losses. However this is far from proven. Those who accept the appetite
dulling effect of ketosis ( and there are doubts about this effect) stress the
discomfort of the intermittent method. As a result of either or both the weight
increase and/or the effect on appetite, there is a greater risk of an
unsuccessful outcome as a result of people dropping out. Moreover, practical
experience of substantial weight losses by continuous VLCD use over many months
has shown no undesirable effects.
2.7 Long-term
efficacy
Very low energy diets per se cannot
achieve long-term weight control any more than can any weight loss method. The
only way to achieve long-term weight control is by a fundamental change in
lifestyle (eg regular exercise, smaller meals, lower fat content).
From the
earliest studies of, for example, Stunkard & McLaren-Hume (1959) it has been
clear that, in practice, the vast majority of those who lose weight by whatever
means (reduced food intake, formula diets, exercise, behaviour modification,
drugs etc) are back to about their pre-dieting weight within 1-5 years. In
general terms it appears that bariatric surgery, though it has mortality and
morbidity in excess of medical management may have better long-term results on
weight control. However a recent paper (KIein et aI 2000) stresses that when a
successful cohort of surgical and medical weight losers are compared, the
differences may not be all that great in psychosocial terms.
The obesity
literature now abounds with reports of attempts to effect long-term maintenance
of reduced weight and to define the factors that can predict the chances of
success in the individual (e.g. de Pue et al 1995, Pasman, Saris &
Westerteerp-Plantenga 1999; Karkeila et al, 1999 each looking at different
aspects)- There have been some recent studies of the effect of a lipase
inhibitor (Orlistat e,g, Rossner et al 2000) which appear promising, but there
are so many examples of early enthusiasm and later disappointment in this field,
that it appears wise to exclude these observations for the present. Moreover
there are some unpleasant side effects associated with the use of Orlistat and
this may preclude the long-term use of this preparation.
The current
views on the principles which lead to the best long-term results appear to
be-
·
It is vital to manage excess
weight as a progressive chronic disorder The longer and more intense is the
support and counselling the better is the result
·
Long-term support and
counselling by a trained non-professional can be just as or even more effective
than professional care (e.g. Wing & Jeffery, 1999). What matters is
willingness of the advisor to provide long-term adequate firm support with
empathy. Time and patience are essentiaI.
·
If the reason for the
overeating can be established and alternative strategies established this
appears to help
·
Reduced fat intake, appetite
reduction (including appetite suppressants e.g Apfelbaum et al 1999) are common
strategies, but perhaps of greater importance is the encouragement of adequate
regular aerobic exercise.
·
Self-help groups appear to
be of value for some people (Andersen & Grimsmo 1999)
·
There is no single technique
which works with everybody and tailoring a selection of procedures to the
individual is to be encouraged.
During the 1980s
there was quite a large literature, particularly in the USA and among those who
favoured behaviour modification, suggesting that the use of VLCD reduced the
potential for long-term maintenance and this view was represented strongly in
the 1990 SCF Report. However more recent studies show that the results of
education towards more exercise and smaller more appropriate food intake can be
achieved during and after VLCD use at least as well as with other
diets.
Very low caIorie diets have been reported
to be a valuable component of long-term weight reduction and control regimes
(Dietz & Greenberg, 1985; Palgi et al., 1985; Wadden et aI., 1986; Kirschner
et aI., 1988; Sikand et al., 1988; Hovell et al, 1988;
Wadden et al., 1988; Miura et al., 1989.
Cox et aI_, 1989. Wadden et al., 1989; Niemi et al., 1990; Anderson &
Brinkman, 1990. Atkinson, 1990; Donnelly et al., 1991;
Brownell, 1991; Cox et aI_, 1991;
Anderson et al., 1991; Brownell & Wadden, 1991;
Wing et al., 1991; Wadden et al_, 1992;
Anderson et al., 1992; Atkinson et aI., 1992; Blair, 1993 inter alia). Indeed
several studies over the past five years suggest that the long-term results may
be superior when a VLCD is used as one feature of the process which leads to a
lifestyle change (Quaade & Jensen 1995, Wadden & Frey 1997, Andersen et
al 1999, Apfelbaum et al 1999), though this is far from proven. One interesting
feature is that a substantial number of trials in the last few years of the
twentieth century used VLCD as their diet component without referring to it as a
VLCD. This suggests that VLCD are becoming accepted as equivalent in safety to
any formula diet but as more effective. Even more interesting is the fact that
some of the behaviour modification groups who wrote most vehemently against VLCD
in the 1980s are now using and advising VLCD as the diet component of their
overall management.
When the
revision of the original 1998 report to the SCOOP Working Group was first
started, the aim was to try to determine by an analysis of the literature
whether the long-term results using VLCD are at least as good as those with
other energy reduced foods. F or the present this has been abandoned
because the level of variation in the length and intensity of the support and
counselling, the food advice, the form and intensity of the exercise inter alia is so substantial. Added to this
there is considerable variation in the drop-out rate and how the drop-out
information is handled in the analysis presented in the original
papers.
However as a
result of a request from the working group we have examined further the question
of a comparison of the long-term results with VLCD compared with the results
that can be achieved in the long-term using other methods and other diets. This
examination confirmed our previous view that it is impossible to find in the
literature valid information on
which a reasonable appraisal can be based that would withstand even minimal
critical analysis.
We would
specifically draw attention to the following table showing a selection of the
various factors identified in the literature as influencing the long term
efficacy viz:
|
As to:
|
Variation
|
|
Pre-treatment data
|
Expressed
in different units: kg, kg excess, BMI, %excess,
Mean of
group (?SE), median, range,
Exact
definition of normal weight is not given
Educational and work
status.
Probable
reason for excess weight
|
|
Treatment
|
How deal
with dropouts – sometimes not even mentioned
How long;
? goal set; ?what form of diet: ?food, formula, ? calories, ?macronutrient
levels (sometimes data not given)
?
behaviour modification –if so what and how frequent. ?eating cues,? Rate
of eating,? Record keeping, ?rewards given – if so what and
when
?
counselling – if so by whom, frequency, nature length etc
?
psychiatric appraisal and how followed
? diet
education – if so how much, what etc
?
medication – if so what. Frequently not stated at all
? how good
is compliance actual loss/week cf expected
? exercise
– if so what type, how often, ? compliance
?any time
in hospital/clinic – if so conditions applied
|
|
Weight
loss – how expressed
|
? as %
excess weight change; ? as BMI; ?as median of group, ?as mean of group
(?+SE); ? as kg change
Some times
the weight loss is expressed in different units from the pre-treatment
situation making it impossible to translate one to the
other.
|
|
Change to
maintenance
|
? sudden;
?gradual change if so details of rate of change;? Specific foods/food
types allowed or restricted;
|
|
Maintenance
|
? goal
setting ? target – if so what and how expressed
?
behaviour modification maintained – if so what and how
?
counselling – if so how often, for how long, by whom etc
? seen at
all . ? contacted by telephone – by whom, how, frequency etc
? exercise
– if so ? advised or undertaken with group, what type, how frequently, how
controlled etc
? dietary
advise – if so in form of avoidance, ? strict diet. ? calorie counting,
?”sensible eating pattern” etc
Formula
intake allowed as component – if so under what conditions, ? redieting
allowed as necessary during follow up
? regular
weighing – if so what frequency, under control or at home, ? what to do in
event of change
? medicine
– if so what type and how controlled
Spouse/family/lay friends etc
involvement ? group care
Educational and work
status.
Has
probable reason for excess weight been dealt with
adequately
|
|
Treatment
|
How deal
with dropouts – sometimes not even mentioned
How long;
? goal set; ?what form of diet: ?food, formula, ? calories, ?macronutrient
levels (sometimes data not given)
?
behaviour modification –if so what and how frequent. ?eating cues,? Rate
of eating,? Record keeping, ?rewards given – if so what and
when
?
counselling – if so by whom, frequency, nature length etc
?
psychiatric appraisal and how followed
? diet
education – if so how much, what etc
?
medication – if so what. Frequently not stated at all
? how good
is compliance actual loss/week cf expected
? exercise
– if so what type, how often, ? compliance
?any time
in hospital/clinic – if so conditions applied
|
|
Weight
loss – how expressed
|
? as %
excess weight change; ? as BMI; ?as median of group, ?as mean of group
(?+SE); ? as kg change
Some times
the weight loss is expressed in different units from the pre-treatment
situation making it impossible to translate one to the
other.
|
|
Change to
maintenance
|
? sudden;
?gradual change if so details of rate of change;? Specific foods/food
types allowed or restricted;
|
|
Maintenance
|
? goal
setting ? target – if so what and how expressed
?
behaviour modification maintained – if so what and how
?
counselling – if so how often, for how long, by whom etc
? seen at
all . ? contacted by telephone – by whom, how, frequency etc
? exercise
– if so ? advised or undertaken with group, what type, how frequently, how
controlled etc
? dietary
advise – if so in form of avoidance, ? strict diet. ? calorie counting,
?”sensible eating pattern” etc
Formula
intake allowed as component – if so under what conditions, ? redieting
allowed as necessary during follow up
? regular
weighing – if so what frequency, under control or at home, ? what to do in
event of change
? medicine
– if so what type and how controlled
Spouse/family/lay friends etc
involvement ? group care
Educational and work
status.
Has
probable reason for excess weight been dealt with
adequately
|
|
Results
expression
|
How
followed up ? telephone, ? questionnaire; ? seen – if so is advice given
at same time, frequency etc
How deal
with dropouts during follow up.
How is
result defined ? in relation to target; ?in relation to lowest
weight/weight at end of diet phase. How dealt with when gradual change to
maintenance.
See also
other problems under pre-treatment and during
treatment
|
As if this
situation were not daunting enough, the individual papers do not attempt to
specify even a limited proportion of these confounding features, nor is it
possible to find standard answers to even a limited list.
However, while
bearing all the concerns about validity in mind, I have taken a random selection
of the results and expressed them in the form of graphs. Since it seems that the
greatest relevance lies in the percentage change from the original weight that
is achieved at each stage, we have expressed the graphs in this form so far as
possible. We have accepted the figures as reported in the original paper and not
attempted to correct for dropout level (where this is stated) since there are
various ways by which dropouts could be corrected.
Specifically we
have selected papers (see figures 2.2 to 2.10) which indicate that while the
general proposition is true, namely that stopping control of the subjects means
a return to their original state, demonstrate that there are a many studies in
which this has been avoided, by long-term close control. Moreover even in those
groups in which recidivism is the rule, there is a proportion of the population
who have sustained a substantial weight reduction. The information which has
been presented, shows we believe that the long term results have nothing to do
with the precise means of weight reduction or maintenance, but depend on the
amount of effort that is put into long-term management. This is scarcely
surprising for a psycho-social disorder.
Figure 2.2. A
diagram taken from Hensrud et al (1995) showing the effect of a study with an
800kcal food based diet in moderately overweight women. At the end of the
dieting period no further action was taken until the subjects returned at the
end of 4 years. The result is compared with a control group of normal
weight women to show that the normal weight does rise with time. The failure of
weight maintenance is typical

Figure 2.3.
Diagram from Bjorvell & Rossner (1985). This compares a control group who
were given instructions about how to lose weight but then left to look after
themselves. The next (dotted) line is that for a food based 600kcal food based
diet . In the maintenance phase, the subjects could take part in a regular
advisory programme if they wished The lowest (dashed line is that for jaw wiring
followed by a regular voluntary advisory service . Note that with the advisory
service there was a reasonable weight maintenance, in this study apparently
better for VLCD than for jaw wiring
Figure 2.4 This
is a diagram based upon the information in the paper by Anderson et al (1992).
They used a 500kcal VLCD and achieved a good weight loss. The subjects were
encouraged to undertake a weekly advisory programme during the 24 month follow
up with self monitored exercise , but only a proportion did.
Figure 2.5
This is a diagram from the Pasman et al (1999) study. This treated the whole
group with a 460kcal diet for two months. All subjects took part in an endurance
programme for the first four months. Then one group (solid) continued with the
exercise for the rest of the period while the others acted as a control
group. In this study there was no apparent difference as a result of the
exercise regime used.

Figure 2.6
This is a diagram from the study by Torgerson et al (1997). It compares a non
VLVD group (hypocaloric food diet throughout) with a group who took VLCD
(400-500kcal) for 12 weeks followed by a hypocaloric diet for the rest of the
period. The final result for women shows no difference, but that for men a
greater weight reduction and then a lower end point. It is interesting that men
show better results in most of the papers. This diagram shows that there are
specific reasons for different responses, not just the use of VLCD

Figure 2.7 This
diagram by Miura (1989) shows the effect of VLCD alone, behaviour modification
alone and a combination of the two This particular behaviour modification
programme appears to be effective – others do not.
Figure 2.8 This
is a diagram from Ohno et al,(1990). Like Figure 8 it shows an effective pattern
with VLCD plus behaviour modification but not with VLCD alone.

Figure
2.9 This is the study by Pavlou et al (1989). This study, in
contradistinction to others shows a beneficial effect of exercise on the
long-term results with both 800 kcal food and formula diets and with a 420kcal
VLCD. I am puzzled that the non exercise hypocaloric food diet was so effective
in reducing the weight.
Figure 2.10 This
diagam comes from Dittchuneit et al (1999) who compared the effect of either a
food based diet (1500kcal approximately) or a diet in which two of the meals
were replaced by a formula diet for 3 months. For the 24 months
maintenance phase all the subjects consumed a maintenance programme diet which
substituted one of the three meals by a formula diet. There was a monthly
weighing programme but no behaviour modification was attempted..
SECTION III.: RECENT
SCIENTIFIC STUDIES WHICH HAVE PRODUCED A BETTER UNDERSTANDING OF THE PROPERTIES
OF VERY LOW CALORIE DIETS.
During the 1980s two
fundamentally opposing views developed concerning the nature of the body
composition changes which occurs when weight is lost and the influence exerted
by the composition of the diet on the body compositional changes. This is
exemplified by the differences to be seen in the COMA (1987) report and that for
example in the SCF (1990) and Codex Alimentarius (1995) reports.
The first view was that
propounded by Webster et al (1984), Garrow et al (1985) which supports the older
view if James et al (1978). This held that when weight is lost as a result of
any energy deficit
with a diet which provides adequate macronutrients, be it at 400 or 1200kcal
intake per day, protein is naturally and necessarily lost at the same time as
fat, the accepted proportion being about 75% fat: 25% protein.
The alternative view,
which depended largely on the observations of Forbes (1987) was that the
proportion of fat to protein in the weight which was lost varied depending upon
the proportion of the fat in the body. Thus it was held that for those who were
very obese a substantial proportion of the weight loss consisted of fat while
for those of lesser levels of excess weight (and therefore fat) there was a
significantly higher proportion of lean fat loss. This would have the effect
that not only would there be increased danger of protein deprivation in those of
lesser excess weight, but in this group the loss of the additional lean mass
would also have a greater lasting effect on future ability to maintain the lower
weight due to the reduction in the basal metabolic rate. It was further argued
that in the overweight the loss of lean body mass would be replaced by fat
during re-feeding.
These alternative views
have such a vital effect on our understanding of the body composition effects of
dieting that it was felt imperative to examine the extensive recent literature
on the subject to determine where the truth lies. To this end the following
matters were reviewed.
1.
The level of accuracy and
reproducibility of the various techniques which have been used for the study of
body composition changes.
2.
The studies that have been
undertaken on body composition changes during weight loss and their
interpretation.
3.1 Examination of the body composition determination
methods.
3.1.1 Reliability of the analytical methods.
There are now a
substantial number of papers which deal with the reliability of various
analytical methods for determining the composition of weight losses during
dieting. A qualitative overview of these is given in the paper by Lukaski (1987)
(Table 3.1).
3.1.2
Kjeldall method for
nitrogen determination
One of the
methods not considered in the Lukaski paper is that of nitrogen balance by
Kjeldall analysis, a method which was widely used in earlier studies including
some of those quoted by Forbes. Because it was so widely used and quoted in the
1980s literature, a study of the reliability was undertaken in Cambridge.(Kreitzman
& Beeson 2001). This
serves well as an example of one of the difficulties in the whole body
composition area:
“Until recently the
“Kjeldall method” of nitrogen determination was the only method for direct
measurement of protein balance. There are a substantial number of potential
errors arising, for example from inappropriate corrections for unmeasured
nitrogen intake and loss. However less has been published about the reliability
of the method itself and it was therefore felt desirable to check
this.
Samples (from 24 hour
collections of urine) from eighteen subjects who were undertaking a VLCD weight
loss study were submitted for analysis to a widely recognised and extensively
used commercial laboratory. The results, shown in (Figure 3.2) as the left hand
(unshaded) blocks represented a single analysis for each sample.
Each sample was at the
same time pipetted in triplicate into sample bottles and labelled randomly as 54
sequential samples. These were then submitted blind to one of the senior UK
academic laboratories whose results have figured extensively in UK nitrogen
balance studies over many years. Each sample was analysed in duplicate by the
laboratory and the results are presented as an average (shown darker
hatched on the charts (Figure 3.1).
When the code was
broken, the differences between the academic and commercial laboratories on the
same sample were substantial, with each commercial figure representing a
substantially higher daily protein loss. However even more surprising was the
variation between identical samples tested blind in the same academic
laboratory. It is important to stress the importance of the size of the
differences within this laboratory. In the worst case, these differed by as much
as 5g nitrogen per litre. This would be interpreted as more than 30g protein
lost per litre urine
Figure 3.1 The results of the Cambridge study of the
reliability of the Kjeldall measurement of nitrogen balance. For details see the
text.
In the particular
dieting study, the twenty four hour samples that were being analysed generally
amounted to 3 litres total volume. Therefore a difference of 5g/litre would have
meant differences of about 100g/day of lost protein, purely on the reliability
of the method in the laboratory. It is clear that such a difference would render
the nitrogen balance meaningless.
It is fully accepted
that this just represents the results in one laboratory, albeit one of the
reputed best in the UK. The only interpretation which should be applied is that
for any laboratory presenting nitrogen balances based on micro-Kjeldall
estimations, there should be a blind study at regular intervals of the
reliability of the method in their laboratory and preferably a blind audit
across a group of laboratories”.
In this respect
it is worth pointing out that the problem with a graph of the Forbes/Prentice
type which takes results from various laboratories, at different times, is that
the cross reliability between laboratories is largely or completely unknown.
This concern also applies to the Ballor & Poehlman (1994) widely quoted
paper on the influence of exercise on the FFM loss, since this paper utilises
information from various laboratories the cross reliability of which is
unknown.
3.1.3 Reliability of indirect methods of
estimating the body protein economy.
It is important
to stress that the vast majority of the methods used in papers which purport
to determine protein balances during weight loss do not measure nitrogen,
but set out to estimate a representation of the protein content of the body from
other measurements. The estimate which is most widely presented used to be
called “lean body mass (LBM)” but is now better called “fat free mass
(FFM)”.
Contrary to
popular medical belief FFM does not represent the protein component but consists
of at least 6 compartments (intra-cellular water, extra-cellular water,
glycogen, bone, minerals, protein). Each of these compartments can change
independent of the other to a greater or lesser extent during physiological and
pathological conditions (including dieting). For example, the physiological
conditions which have a profound effect on indirect body composition estimations
include:
Changes in glycogen stores which result from pre-study food choice
Hormonal changes e.g. the menstrual cycle and menopause; stress; insulin
states
Exercise
Ambient temperature
Inactivity – not only bed rest but also restriction e.g. plaster cast on a
limb.
It is important
to stress the importance of the glycogen compartment in this whole discussion.
The glycogen store itself is about 400-500g, but each g of glycogen has
associated with it between 3 and 5 g of water. Hence with dieting (or
re-feeding) there will be a change in the first few days in the glycogen
compartment amounting to anything up to 2kg. Thus any current indirect
measurement of body compositional change must take account of this substantial
component. This particularly applies to the first few weeks of dieting (or
re-feeding). This is why it is vital to ignore studies of less than about 4
weeks and also to ignore those in which the post-diet determinations have been
made after even a brief period of “maintenance”.
There are
several older studies that have investigated the variations from one technique
to another (e.g. Yang et al, 1977; Vaswani et al, 1983; Garrow, 1990) However
during the past 10 years a substantial literature has been published on
technical aspects of neutron activation analysis of various chemicals, a
substantial proportion of these papers emanating from the Heymsfield group. This
is currently the only method by which chemicals within the living body can be
measured directly. Among these chemicals is nitrogen. Neutron activation can
determine directly the nitrogen status within the body. Even then it can not
measure the protein economy itself since protein is only one of the nitrogen
containing body components, albeit the largest one. Unfortunately neutron
activation analysis is expensive and there are relatively few units which can
currently undertake this determination. In consequence, though neutron
activation analysis is the current “gold standard” it is still necessary to rely
heavily on indirect estimates of the body composition. Interpretation of the
indirect methods must be guarded and the assumptions questioned
thoroughly
As a consequence
it is important to determine not only the reliability of these various methods
in their own right but how far they cross correlate, one with the other, not
only under stable conditions but under variable physiological and experimental
conditions. There have been many recent papers which have reported such cross
comparisons though usually with only a few methods in any one study. These cover
studies in normal humans, the aged etc. However one study in the USA (Albu et
al, 1992), one in the UK (Kreitzman et al, 1993) and one in Spain (Valtuena et
al, 1995) are directly relevant to the present situation and appear to be the
best to indicate factors of current importance.
The Albu study
(which comes from the Heymsfield group), looked not only at various recent
methods, but also how these would be converted to FFM estimates, using different
equations and different numbers of compartments. They studied 10 dieters, taking
a 600kcal VLCD for 24 weeks and Figure 3.2 shows the dramatically different
estimates for fat and FFM that emerge in each individual dieter when different
study methods are used. It is important to note from this figure that the
variation is not uniform for any individual method (look, for example at the
figures for 40K water dilution (2C-TBK) compared with those for
tritiated water dilution (2C-HD)).

Figure 3.2. Effect of different methods of
determination on the estimated fat loss (from Albu et al, 1992)
In the Kreitzman
et al (1993) study, not only was the change in body composition of the eleven
dieters using a 405 kcal diet for 10 weeks measured by twelve different
observations, but for four of the methods, studies were made in entirely
independent units, namely:
Futrex
3 laboratories
TBK
2 laboratories
Skinfolds 2
laboratories
Impedence 2 laboratories
Thus this study
provides information on both the reliability and reproducibility of the
individual methods of indirect estimation but also cross laboratory
consistancy.
One method of
demonstrating the degree of variability within methods and between methods is to
calculate the FFM changes for each, the ratio DFFM/DFAT and the mean fat weight i.e. the
values used for the Forbes and Prentice diagrams. The ratio which would arise
for each subject using each estimate is shown in the graphs in Figure 3.3 (next
page)
Once again while
the variation in the means is not very great, the individual variations are
large and as irregular as those of the Albu study. With such individual
variability it is clear that it is
Figure 3.3 The results of the study of the
DFFM/DMean Fat Wt ratio in 10 of the 11
subjects who undertook the experimental 10 week VLCD diet. The body composition
of each of the 10 subjects was estimated with 8 main methods (many in
duplicate/triplicate in different units). The details of the studies are to be
found in “The Swansea Trial” Eds Kreitzman SN & Howard AN Smith-Gordon &
Co Ltd 1993. Note that the eleventh subject is not included because she was not
able to undertake the densitometry measurement.
Subjects
1,2,4,5
Subjects
6-9
Subjects
10 –
12
not possible to
reliably recalculate the estimate in any individual patient for one method on
the basis of another method.
The third study
is that of Valtuena et al (1994), graphs showing the results of which are shown
in Figure 3.4. Their results are very similar to those of both Albu et al and
Kreitzman et al, though with fewer methods studied.
Figure 3.4 The results of a study by Valtuena (1995)
of the DFFM/DMean Fat Wt ratio determined in nine
dieters, each studied by three different methods.
It was hoped
that it would be possible to determine whether there was any correlation between
these studies to indicate whether any characteristic of the subject might show a
correlation with deviations in an individual method. Unfortunately it was not
possible to do so because of major differences in the methodology. Indeed it was
not possible to use the Albu data further because it included a variable
maintenance period (24 – 33 weeks). There was an extra problem in further
analysis of the Albu study because only 7 of the 10 dieters were studied post
diet, but the paper does not indicate which they are.
An overall
representation of the variation which derives from the use of different study
methods is shown in Figure 3.5
Figure 3.5 Comparison of the body composition
results using five different methods in four different studies. Densitometry
results are taken as 100 and the results of the other methods expressed as a
proportion of these.
In part the
different results given by the various methods may be explained on the basis of
different degrees of obesity. Thus Gray et al (1989) showed that when the body
fat was over 48% of the total weight, impedance overestimates FFM when compared
with the results from densitometry. In part it depends on other physiological
variables which can change, with time in the same person. For example the
observations recorded by de Groot et al (1989) using diets of very similar
composition show wide fluctuations in the DFFM/DWt ratio (0.09, 0.37, 0.18, 0.47; see
record 24A to 24D in the summary table ***).
Other studies
that have examined the variation in the FFM which results from the use of
different indirect methods include Murgatroyd & Coward (1989); Heymsfield
& Waki (1991); Ballor & Poehlman (1994); Houtkooper et al (2000); Piers
et al (2000).
3.1.4 Variation introduced by different
formulae for conversion using indirect methods.
From what has
been written here it should be clear that each of the indirect methods for
estimating FFM require fundamental assumptions to be made in order to calculate
FFM (or fat and hence FFM by subtraction). The body compartment which is
determined and some of the assumptions that are made for representative indirect
methods are shown in Table 3.2.
Table 3.2 The compartment which is
determined and some assumptions that are made for some of the common body
composition estimation methods.
|
|
Measures
|
|
|
Tritiated
water
|
Exchangeable body
water
|
Constant hydration
of FFM (1)
Stable hydration
state (2)
Oedema fluid
(3)
|
|
40K
|
Body potassium
pool
|
Dietary intake of
K uniform (e.g. milk, fruit etc) (4)
Constant ratio of
K/N (5)
Uniform body
terrain (6)
|
|
Hydrodensitometry
|
Average body
density
|
Very sensitive to
hydration (1)
Water confident
(7)
Dietary status
2)
Sensitive to
bladder and gut contents
Variable equations
which do not always agree
|
|
Impedance
|
Total body water
space
|
Constant
hydration of FFM (1)
Stable hydration
state (2)
Oedema fluid
(3)
|
|
Skinforlds
|
Local fat
deposition
|
Uniform fat
distribution – subject variability
Does not measure
visceral fat
Constant hydration
(1) (2) (8)
Operator
consistency
|
NOTES
1)
Constant
hydration of FFM can not be assumed since total body and compartmental
fluid status is variable at different stages of diet and also varies from
subject to subject. The test converts TBW into FFM based upon the assumption
that FFM is 73% water which is not universally true
2)
Stable
hydration state within and between subjects is assumed and is not true under
different study conditions. Hydration is influenced not only by the intake and
excretion of fluids but also by food, hormones, temperature, activity levels,
drugs etc both before and during any study.
3)
Oedema
fluid is different between subjects especially when obese subjects are compared
with the non-obese. Loss of this fluid may be sensitive to macronutrient
intake.
4)
Dietary
potassium intake will reflect in 40K measurement, e.g in study of
formula diet in which the calories are raised with milk to compare with lower
calorie water. Milk is potassium rich which is measured in total body potassium
pool and would wrongly suggest increased FFM.
5)
Many
studies show that potassium can change independently of nitrogen. Changes in
fluid balance will change potassium without any change in nitrogen.
6)
Terrain-
The measurement of body potassium assumes a constant source to detector distance
and uniform absorption path. Human bodies do not comply, especially when they
are changing shape during weight loss. Also varying fat distribution will
influence readings.
7)
Water
confidence. The test involves underwater weighing of the subject in a confined
tank and if subjects are obese, external weights are needed to keep subject
submerged. Total exhalation is required. The procedure is less problematic in
no-obese subjects.
8)
Oedema
fluid contributes to weight and loss of this fluid will change body weight by a
greater proportion than that shown by skinfold measurements, not least because
the areas where skinfold measurements are made are not those where oedema fluid
would be expected to be marked. This will therefore suggest higher FFM loss per
weight loss but not related to a loss of protein
But even this is
not the limit of variation because many of the estimates include “correction
factors”. These are not the same from one study to another, even
when the same method is used (as an example see Table 3.3.)

Table 3.3. The effect of different prediction
equations on the conversion of hydrostatic measurements to body fat estimates
(from ***)
But even without
variation introduced by the use of different formulae, there is evidence that
the calculations can not be applied across different levels of obesity. Thus
Lohman (1977) showed that for subjects with over 30% fat, the Siri equation for
the calculation from densitometry measurements yields higher values for FFM that
does that of Brozek.
3.1.5
Summary of
the reliability of composition estimates.
To summarise the
situation, the accuracy of each method of body composition estimation depends
upon:
·
The limit of the reliability
and reproducibility of the method per se
·
Accuracy of measurement in
the individual laboratory
·
Biological variations
influencing the interpretation of indirect methods when these actually measure
independently variable body components
·
Different formulae for
converting the observations into a measurement of reputed fat mass, fat free
mass etc.
·
Variation of conditions
within and between the studies
It must be
appreciated that for weight loss studies these problems are further complicated
by the fact that the tests are undertaken both before and after the diet. Each
has its own level of inaccuracy and each is influenced by physiological
variables, including those that arise from endocrine changes resulting from the
diet and the stage of the diet itself (e.g. first week of
re-feeding).
Even then there
are further complications, for it has been demonstrated clearly by Saris that
exercise during dieting can influence the preservation of lean body
mass.
3.1.6 Significance of these variations in
relation to the Forbes/Prentice graphs.
If every single
point in the Forbes/Prentice graph was based upon a determination of the same
body component using the same technique and converted to FFM using the same
formula, there would still be the problem that results from individual
variation. However the situation is far less clear than this. Of the studies
quoted by Forbes (1987) and Prentice et al (1991) as the source of their data
for the graphs which we have examined carefully, the data is probably derived
from the following techniques
Densitometry (some variation in
techniques)
16 studies
40K counting (with
variations)
4 studies
Skinfold
(various)
3 studies
Impedance
(various)
3 studies
IVNAA
1 study
We have used the
words “probably derived” because some of the studies have used more than one
technique and it is not clear which result has been taken for the
Forbes/Prentice graph. It has been assumed that when there was a densitometry
estimate available this was the one that was used, but there is no direct
evidence that this was the case.
On the basis of
what has been presented above, it is submitted to the Working Party that, as
presented, doubt must be cast on the accuracy of the overall graph as shown in
Figure 11b of the Prentice et al (1991) (see Figure 3.6 of this discussion
paper). That graph was based on different indirect methods of estimation,
undertaken in different laboratories and applying different formulae to derive
the body composition.
Figure 3.6 Figure 1 from the Prentice et al (1991)
paper which the Working Party asked to be re-examined.
3.2 Re-examination of the old data and examination of new
data relating to body composition changes
3.2.1
Re-examination of
the Forbes/Prentice graphs.
Despite all the
problems that have been identified, it appeared to be desirable to examine each
of the papers cited by Forbes(1987) and Prentice et al (1991) to determine the
method used and other relevant information.
In addition a
search has been undertaken for other relevant papers over the period from about
1960 to 2000. Over 100 papers which were available for detailed analysis could
be identified.
From these we
have attempted to identify those studies which must be eliminated because they
were invalid and to indicate why (Appendix 4). Ideally only those studies should
be included which are based on formula diets, the exact composition of which
could be verified. Unfortunately this removed almost all the studies of
800-1200kcal diets since the vast majority of these are food based. We therefore
modified the criteria maintaining a category based on the following
criteria
formula based diets for which the composition was clear and which
were
studied for 4-16 weeks without
interruption,
with either no exercise or low level
exercise,
where the rate of weight loss per week
suggested reasonable compliance
and densitometry determinations were
available
These are marked
“Accept” in Appendix 3.
We also added a
further criterion (marked “Provisional” I Appendix 4) for
food based diets between 800 and
1200kcals/day, which were
studied for 4-16 weeks without
interruption,
with either no exercise or low level
exercise,
where the rate of weight loss per week
suggested reasonable compliance
and densitometry determinations were
available
There were a
certain number of these studies which were quite clearly inappropriate
(hydrolysed collagen diet, starvation, use for only a few days etc) and these
have been totally rejected. For the remainder, including those that have been
rejected for other reasons (e.g. method of estimation of the composition) we
have shown all the actual raw data, the basis of the calculations and the
DFFM/DWt ratio and mean fat weight in Appendix
4. From this table it was possible for any member of the Working Group to check
the data. They can then determine whether they feel that the plots of
DFFM/DFAT and mean fat weight which have
been made are valid. The ratios and mean fat weight of those studies that have
been regarded as “acceptable” and “provisional” as bold in this table to make it easier to
distinguish them.
It is
disappointing to find how few valid observations are available from some 40
years of studies worldwide. Of more than 60 papers examined only about 20
contain valid data. This is clearly the only data on which we can try to
determine whether
the FFM component of weight loss is dependent on the body fat mass.
the use of VLCD produces a higher FFM loss than does an 800-1200Kcal
diet.
From this
“valid” data we have shown on separate Figures (Figures 3.7 and 3.8 – next page)
the ratios plotted against MFW for the use of formula based VLCD 400 to 800Kcals
(Figure 3.7) and formula and food based diets between 800 and 1200 kcals (Figure
3.8). We have also plotted the information for the individual dieters in
those studies (Deurenberg 1989: Kreitzman & Howard 1993; Valtuena et al
1995,) in which there are enough observations at various body fat levels
(Figures 3.9, 3.10 and 3.11 – two pages on).
On the basis of
the information given in Appendix III and plotted in Figs 3.7 to 3.11 it is
submitted that there is no current evidence for either of the above widely
publicised views, namely that the composition of the weight which is lost
depends on the body fat level or that VLCD produce a higher proportion of FFM
loss that do higher energy providing diets.
Hence there is
no evidence that VLCD are more dangerous than other diets when used in the
overweight as opposed to the obese. We have sought to determine whether these
views can be supported by statistical analysis but the data is too limited. In
any case the use of statistical methods must be suspect when the data is liable
to such a high level of error.
The figures
which follow have not been re-labelled from those presented to the Working
Group.




3.2.2 The body composition studies expressed in
terms of BMI status.
In the above diagrams relatively little
of the information has been expressed in terms of the original or finishing BMI
level, but information expressed in this way was requested by the Working
Group.
Unfortunately, the body composition data
(by any method) expressed in terms of BMI, are not available for all the
studies. Forbes expressed his results in terms of mean fat weight and most
subsequent authors followed this pattern. However, if it is accepted that a MFW
of 30kg is broadly equivalent to a BMI of 30 then it is clear from Appendix 4
that there are a substantial number of individuals in the range <30 MFW for
diets of <400kcal, 400-600kcal 600-800kcal and above 800kcal.
For some of the studies it is possible to
examine the DFFM/DWt ratio for individual subjects above
and below MFW 30. Therefore although it is not possible to compare with other
studies (due to different methods), it is possible to assess the situation
within the same study. We would specifically draw attention to the fact that not
only do these cover patients whose pre-treatment BMI (or MFW) is below 30 but it
is clear from the data presented that some at least of the subjects were reduced
to BMI levels between 20 and 25
3.2.3
The body
composition studies expressed in terms of the energy value of the
diets.
The data in Appendix III covers a wide
range of diet energy content viz:
|
Energy
content
|
Number of
studies
|
|
<400
|
1
|
|
400-600
|
4
|
|
600-800
|
1
|
|
>800
|
11
|
|
Various
|
2
|
There is no indication that the energy
value of the diet used influenced the body composition changes with weight
loss
3.3
The Keys (1950)
Minnesota Study – an appraisal
This study, which is always quoted
concerning the effect of “semi-starvation” clearly influenced the Forbes
analysis of changes in body composition with changes in body weight during
dieting.
It was undertaken on a group of 32 young
male volunteers. At the start of the study the mean BMI was 21.9. As a result of
24 weeks dieting this was reduced to a mean of 16.9. Body composition studies
were undertaken at time 0, 12 weeks and 24 weeks by hydrodensitometry. The exact
technique differs somewhat from modern methods and the results can not be
compared directly with those quoted in Appendix 4.
The ratio of DFFM/DWt loss for the first 12 weeks (BMI
change from 21.9 to 18.7) is 0.63. The ratio for the second twelve
weeks (BMI change from 18.7 to 16.9) is 0.57. Thus the lower the BMI the less
was the protein lossas opposed to the opposite determined by Forbes.
However it is our opinion that the Keys’
study should be discounted as of no relevance to considerations of VLCD dieting
for the following reasons:
·
The average BMI at the start
of the Minnesota dieting period was 21.7 (i.e. low area of normal) and not a
level at which dieting should be contemplated.
·
The dieting took the BMI
down to average 16.9 (the pictures within the book show how emaciated they
were), the residual fat averaged only 3.4kg according to their calculations and
this is substantially below any target weight for therapeutic
dieting.
·
Three different food diets
with substantially different proportions of fat, carbohydrate and protein were
used on different days.
·
The average energy intake
per day over the 24 weeks and 32 subjects was no less than 1569 kcal, but this
hides a range of means for individual subjects between 1213 and 1833 kcal. The
range between individuals by weeks stretched from 608 to 2095 kcal. The diet was
adjusted individually each week to achieve a theoretical weight loss curve. The
energy value and composition of the diet was changed depending on the previous
week’s weight loss. The adjustment was mainly by additional carbohydrate and
hence the glycogen stores would have changed erratically.
·
A high enough energy
expenditure to achieve the required weight loss with the high energy intake was
achieved by daily exercise mainly outside in the bitter cold (Minnesota in
the winter!)
·
“The weight loss was
complicated by clinical oedema and
relative increase in interstitial fluid volume” Keys attempted to adjust
the composition to allow for this fluid accumulation. The adjustment which he
applied changes the ratio for the second 12 weeks to 0.34. This is even further against the
Forbes effect
Interestingly one of the volunteers in
the Kreitzman study had a starting and finishing BMI almost equal to the mean in
the Minnesota study but with a ratio of 0.36, well within the ordinary
densitometry range in that study
3.4
A re-appraisal of the
Forbes and Prentice graphs
On the next page we have reproduced the
Forbes and Prentice graphs as they were shown in their original papers.
(shown as Graphs 3.12 a & b)
However it is clear that the two points
to the far left of each of these diagrams can not represent figures determined
from a regular dieting programme since they represent subjects whose mean body
fat wt is under 10kg (i.e. a sub-normal mean BMI).
If then we accept all the other points on
these graphs as being valid (and it will be recalled that in the discussion
above (page * et seq) we drew attention to problems in accepting them) we can
derive two revised graphs (shown as Graphs 3.13 a & b)
There is then no indication from visual
inspection that there is any increase in the proportion of fat free mass loss at
lower mean body fat levels.
This is not to say that at
Low levels of protein and perhaps
carbohydrate in the diet there may be serious changes in composition of the body
weight loss
At low levels of BMI (below BMI 20) there
may be changes too

Figures 3.12 a & b The original Forbes and Prentice
graphs.

Figures 3.13 a & b. The Forbes and Prentice graphs with the
two left hand points, which can not represent regular weight reduction results
removed
For a better
view of figures 3.12 and 3.13 click here
3.5 Further data relating to body
composition changes during weight loss with VLCD.
There are two extensive individual
studies (Hoie, Bruusgaard and Thom, 1993; Donnelly, Jacobsen and Whatley,1994)
which provide excellent information relating to the question of whether the loss
of fat free mass is greater at a lower BMI level.
In that undertaken by Hoie et al, (1993)
body composition analysis was undertaken by near-infra-red interactance (Futrex
5000). It was conducted on 82 women and 45 men and a 430kcal diet containing
61.5 g high quality protein and 30.5g carbohydrate was consumed daily for eight
consecutive weeks. Dr Hoie has very kindly provided me with the summary of the
original data on which his paper was based, (unfortunately the data on each
individual dieter has been lost in the intervening 10 years). Nevertheless the
information in his original paper and that in the summary tables is adequate to
reach substantial conclusions.
Thus, the proportion of the total group
in the various BMI categories at the start of dieting and after 8 weeks as
calculated from his data is shown in Table 3.4. From this it is clear that as a
result of an average loss of some 3.9 BMI units for women and 4.8 units for men
some 20% of the group came into the normal weight category (BMI 20-25) at the
conclusion of the 8 weeks diet with a further 30% now having a BMI between 25
and 30.
Table 3.4 Number (%) of dieters in each BMI range
at start and end of an 8 week diet (Hoie et al (1993)
|
BMI Range
|
Number (%) time 0
|
Number(%) time 8
wks
|
|
20-24.9
|
0
|
25 (20%)
|
|
25-27.9
|
7 (6%)
|
19 (15%)
|
|
28-299.9
|
19 (15%)
|
19 (15%)
|
|
>30
|
101 (79%)
|
64
(50%)
|
The ratio of FFM/Wt loss overall was 0.25 with
no significant difference between men and women. Without the records for the
individual dieters it has not been possible to construct a scatter diagram of
this ratio compared with the initial BMI but Hoie et al (1993) found that the
ratio did not differ significantly over the whole range from 51 down to 25 (r =
-0.03; P = 0.75). >
The study by Donnelly et al (1994) on the
other hand was conducted only in women (116) using a diet providing
520kcals (protein 50g, carbohydrate 79g) for 12 weeks and with body composition
determined by hydrodensitometry (Brozek et al equation).
For the Donnelly et al study, Table 3.5
indicates the number and percentage of subjects who fell into different BMI
categories before and after the diet. Before dieting the lowest BMI was 27, the
highest 64 (mean 37.6) and with a mean fall of 20.2kgs over the 12 weeks, the
mean BMI level at the end of dieting was 30.2 with no less than 16 (14%)
achieving a normal weight (BMI<25) (range 21.9 – 52.1)
Table 3.5 Number (%) of dieters in each BMI
range at start and end of 12 week diet. (Donnelly et al, 1994)
|
BMI range
|
Number of dieters (time
0)
|
Number of dieters (12
wks)
|
|
20-24.9
|
0 (0%)
|
16 (14%)
|
|
25-29.9
|
9 (8%)
|
48 (41%)
|
|
30-34.9
|
37 (32%)
|
37 (32%)
|
|
35-39.9
|
39 (34%)
|
8 (7%)
|
|
40-44.9
|
20 (17%)
|
4 (3%)
|
|
>44.9
|
11 (9%)
|
3
(3%)
|
Figure 3.13 shows the relationship
between the ratio of the FFM/Wt loss and the BMI level. The mean FFM/Wt loss
ratio was 0.19 (r = -0.9 x 10-7) confirming that there is no
difference in the FFM proportional loss at different BMI levels. It is worthy of
note that the level of compliance to the diet was excellent with only 4 dieters
showing a weight loss per week of less than 1kg. Each of these four with poor
compliance recorded a FFM/Wt loss ratio that was substantially out of line
including both those at the extremes.
Figure 3.13 A scatter diagram of the ratio of FFM to
weight loss compared with the initial BMI in 116 women dieting for 12 weeks on a
520Kcal VLVD (Based on data from Donnelly et al, 1994)
Although the
Hoie et al (1993) study used near infra-red interactance to measure the body
composition, while Donnelly et al (1994) used densitometry, the proportion of
fat lost to weight lost was of the same order in both studies. Moreover the
study by Hoie et al was based on a relatively high daily protein ketogenic diet
while that of Donnelly et al involved a non-ketogenic diet with more modest
protein content.
3.6 Summary of the
body composition study determinations.
From the information derived from the 20
studies involving a relatively limited number of dieters (using VLCD and LCD)
coupled with that from the two extensive studies which examined
ketogenic/non-ketogenic VLCD and the two genders, it can be concluded that there
is no difference in the proportion of fat which is lost during
dieting:
between LCD and VLCD,
between men and women,
between ketogenic and non-ketogenic diets
throughout the whole range of initial BMI levels from about 60 down to
25
and finishing BMI levels in the normal range (20 –25).
3.7 Submission related to the matter of positive and negative
nitrogen balances
In an earlier portion of this submission we have examined the
accuracy, reliability and reproducibility of Kjeldall determinations in general
(Section 3.1.2). Investigation of the current literature in those areas where
there are economic considerations (e.g. studies of protein in animal carcasses
for commercial exploitation) indicate that the Kjeldall method has been largely
abandoned. This is not to say that with appropriate control and care it is not
possible to determine the nitrogen balance by the use of Kjeldall
determinations. However it does stress the need for such careful controls and
means that balance studies which use this technique must be examined carefully
to determine what controls have been applied.
This is particularly relevant in the light of some of the
discussion papers which have been presented to the Working Group concerning the
nitrogen balance during weight loss as a result of dieting. Many of these are
quoted as showing either a positive nitrogen balance or alternatively a negative
nitrogen balance in the early stages which subsequently becomes positive after a
period of some three to four weeks. There is a fundamental problem here.
While weight is being lost with any weight
reducing programme, there is no possibility that there can be a zero, let alone
positive nitrogen balance.
This was established and accepted by the authorities as long ago as 1987 (see
Appendix F of The COMA Report (1987) on the Use of Very Low Calorie Diets
in Obesity). This appendix was prepared by John Garrow in response to the
Cambridge Nutrition calculation of protein losses (see page 38).
It stems from the fact that
when adipose tissue is lost or gained, a significant proportion consists of fat
free mass (FFM). This FFM contains protein. In the calculation given by Garrow
(which uses the proportion 25%FFM/75%fat for adipose tissue) this “allowable”
protein loss (as Garrow calls it) amounts to 4.75% of the total weight lost.
Although there are some differences of opinion about the exact proportion of the
weight lost which consists of FFM the acceptance of this principle implies that
there must be nitrogen loss when weight is being lost. This has been discussed
in detail in an earlier sections of this present paper (3.1 to 3.6). Since this
nitrogen loss is always present in weight loss, we would prefer to refer to it
as “obligatory” rather than “allowable”
Hence what we must look at during
weight reduction is not the nitrogen balance as calculated, but whether nitrogen
losses are greater than the “obligatory nitrogen losses”.
We have accordingly examined as much of the nitrogen balance
literature as we can find to determine whether at a level of 50g of
quality protein intake per day in the form of a VLCD, the nitrogen losses are
greater than the obligatory nitrogen losses.
4. We
have excluded several of the papers because at 50g protein intake per day, they
report a positive nitrogen balance per day even when the matter of the
obligatory nitrogen loss is ignored. These include those of Apfelbaum et al,
1967; Winterer et al, 1980; Blackburn et al, 1975; Bistrian et al, 1977a;
Bistrian et al, 1976; Marliss et al, 1978 ; Bistrian et al, 1977b; Hoffer et al,
1974; Genuth, 1979; Phinney et al, 1988; Vasquez et al, 1985. In these papers
the positive nitrogen balance occurred at various levels of carbohydrate intake
above about 30g available carbohydrate per day.
5. There
is a further group which should be rejected from analysis because the length of
the study was substantially less that 4 weeks or there was no nitrogen balance
or there were obvious fallacies in the design. (Hoffer et al 1984 – No nitrogen
balance provided; Genuth et al, 1974 – No absolute values for nitrogen; Yang
& van Itallie, 1976 10 day experiments only; Baird et al 1974 – Short
periods only with various diets; Aoki et al, 1975 – 7 day experiments only;
Howard et al, 1978 100g CHO – 5 day balance only; Hendler et al 1988- 21 day
only on CHO; Greenberg et al 1976 – not dieting; post operative;
Bistrian 1977 – unable to find paper).
6. We
have equally excluded from the analysis those with a carbohydrate level below
30g/day (since the 1970s it has been known that these levels are inappropriate)
and where the protein level is less than 30g (for a similar reason). (Yang &
van Itallie, 1984 – mixes groups with no CHO and high CHO; Bistrian et al, 1977.
CHO below 30g/day; Marliss et al, 1978 CHO less than 30g; Koppeschaar et al,
1983 25g protein and 25g CHO; Wynn et al 1985 Various CHO values mixed; Fisler
et al, 1982 – CHO below 30g/day; Vasquez et al, 1992 – only 10g CHO/day)
This leaves a total of 15 published papers which can be used
for further analysis, namely:
1.
Howard & Baird, 1977
2.
Wilson & Lamberts, 1979
3.
Hanefeld, 1987a
4.
Hanefeld, 1987b
5.
Ditshuneit et al, 1985a
6.
Ditshuneit et al, 1985b
7.
Alban Davies & Baird, 1987
8.
Wechsler et al, 1984
9.
Wechsler et al, 1984
10.Bistrian et
al, 1981 – 21 days only
11.Vasquez et
al, 1992
12.de
Haven et al, 1980 – 21 days only
13.Morgan et
al, 1993
14.Henry et al,
1986
15.Henry et al,
1986
These are analysed in Table 3.6
Table 3.6 Nitrogen balance
studies (for details see text)
|
Reference
no.
|
Weeks
|
Wt loss /week
|
Prot intake g/day
|
CHO g/day
|
Balance a
|
Balance b
|
Obligatory loss
|
Balance c
|
|
1
|
6
|
2.7kg
|
31
|
40
|
-437
|
-437
|
-643
|
+361
|
|
2
|
4
|
2.4kg
|
31
|
40
|
-602
|
-602
|
-355
|
-70
|
|
3
|
4
|
2.5kg
|
33
|
40
|
-152
|
-264
|
-333
|
-333
|
|
4
|
4
|
2.4kg
|
34.5
|
40
|
-264
|
-264
|
-342
|
+147
|
|
5
|
4
|
2.9kg
|
33
|
40
|
-552
|
-552
|
-432
|
-76
|
|
6
|
4
|
2.7kg
|
33
|
40
|
-433
|
-433
|
-403
|
43
|
|
7
|
8
|
2.0kg
|
33
|
40
|
-490
|
-490
|
-641
|
462
|
|
8
|
4
|
2.9kg
|
50
|
45
|
110
|
-86
|
-437
|
-86
|
|
9
|
4
|
2.7kg
|
33
|
45
|
-323
|
-519
|
-404
|
-43
|
|
10
|
3*
|
2.1kg*
|
46
|
40
|
-433
|
-433
|
-180
|
-349
|
|
11
|
4
|
2.1kg
|
52
|
76
|
-117
|
-201
|
-275
|
-257
|
|
12
|
3*
|
2.7kg
|
50
|
50
|
-569
|
-569
|
-261
|
-569
|
|
13
|
11
|
1.5kg
|
42
|
44
|
-761
|
-761
|
-651
|
-145
|
|
14
|
5
|
2.2kg
|
30
|
40
|
-706
|
-706
|
-408
|
-6
|
|
15
|
5
|
3.2kg
|
30
|
40
|
-1415
|
-1415
|
-650
|
-595
|
Balance a = as presented in
paper (cumulative g protein)
Balance b = as re-calculated
for any additional losses not included in the paper (i.e. nitrogen loss in faeces = 0.7g nitrogen/d = 5g protein
/day; miscellaneous losses = 0.4g nitrogen/day = 3g protein/day)
Obligatory protein loss 0.475% (weight loss –
2.5kg). This is the Garrow Formula (see COMA Report (1987) (cumulative g
protein)
Balance c. The theoretical
balance for an intake of 50g/day protein rather than that used in the paper
(cumulative g protein)
* Note:
with studies less than 4 weeks it is far from clear whether the Garrow
obligatory protein loss formula applies. We have accordingly excluded all the
studies lasting substantially below 4 weeks, but included those at 3 weeks with
this caveat.
It will be seen that for many of these studies the total
protein loss (Balance b) is not much greater than the obligatory loss even at
the lower protein intakes. There are 2 studies of 4 weeks or more and a protein
intake of 50g or more and in both these balance b does not show a greater loss
that the obligatory loss. When a theoretical calculation is made to adjust to an
intake of 50g/day the loss is nearly always no greater than the obligatory
loss.
We fully accept that this is not an ideal presentation. In
previous sections we have already suggested that nitrogen determinations by the
Kjeldall method are suspect. Moreover the re-calculation to an intake of 50g has
no scientific support. Nevertheless there are no current observations of
nitrogen balances determined by neutron activation. Hence, we submit that if Kjeldall determined nitrogen balances
are to be considered (and they are discussed in other papers submitted to the
working group and included in the draft SCOOP Report), then adjustments of the
type given in Table 3.6 are the only possible way of presenting the picture.
3.8 Studies which provide information on the desirable
carbohydrate level.
It is vital to appreciate that the safety of 40g+
carbohydrate is confirmed by the fact that some 90% (45,000) of the patients
studied in the published trials were at daily carbohydrate levels between 30 and
45g. Hence the clinical effects are well known and the safety well established.
with VLCD with carbohydrate levels substantially below 50g/day (but over
30g/day).
The substantial majority (almost
90%) of the published papers which demonstrate the safety of modern VLCD (see
Table 2.1) were concerned with diets containing less than 45g/day carbohydrate.
Such diets produce a mild ketosis in the majority of the dieters. The mean
plasma ß-hydroxybutyrate with 40 to 45g available carbohydrate per day is
1mmol/L with a maximum in a group of 491 dieters tested after over two weeks
continuous dieting 5mmol/L (Tiessen & Weinkove, personal communication).
From the early studies (Baird & Howard, 1974) it has been apparent that when
the available carbohydrate is less than 30g per day the level is inadequate to
prevent mineral losses and increased uric acid levels. However all the clinical
biochemical investigations at levels above 30g/day have failed to show
abnormalities. Moreover, in the United Kingdom and several other countries, the
carbohydrate level for some years was under 35g/day and the practical clinical
results were good at this level. On the other hand there is virtually no
published experience with carbohydrate levels in excess of 50d/day (Table
2.1)
There are two arguments in favour
of a mildly ketogenic diet, namely appetite suppression and a greater sparing of
lean body mass. Search of the literature shows that there is an almost even
split between those who favour a mildly ketogenic one and those who favour a
higher carbohydrate level which renders the substantial proportion of dieters
non-ketotic.
We would submit that unless it
can be shown that there is clear evidence presented that the non-ketotic
solution has substantial benefits for the maintenance of the protein economy, it
would be better to leave it open that VLCD with available carbohydrate levels
above 40g/day are safe. If a higher value is given, it is important to determine
precisely how powerful is the evidence for the necessity, or even benefits of
non-ketotic diets. I note incidentally that the minutes specifically ask that
any evidence showing that above 50g carbohydrate/day is safer than 50g/day
should be circulated, but no such evidence was circulated.
The biochemical argument for the
merit of ketone bodies is that other than glucose, they are the only compounds
that can be metabolised by the brain and indeed are preferentially used by that
organ. Hence when glycogen stores are depleted, under any circumstances, the
production of ketone bodies means that protein breakdown is less necessary to
provide glucose. Thus the phenomenon of protein sparing has been described not
only in starvation, (e.g. Cahill, 1976; Sapir and Walser, 1977) but also under
surgical stress (Williamson et al, 1977; Rich and Wright, 1979; Crowe et al,
1989). We would draw attention to the protein balance data shown in Table 3.6.
This indicates that even at levels of protein intake below 35g/day many of the
papers show that protein losses are no greater that the obligatory losses during
weight reduction by any means. Unfortunately this evidence is not as powerful as
it might be, because there are virtually no observations with non-ketogenic
carbohydrate levels.
As further support for this view,
we would draw attention to the paper by Fery et al (1996). They conclude (page
E829) “The present study, based on the prolonged suppression of FFA and KB or of
FFA alone, suggests that both compounds participate in the conservation of the
protein mass during fasting and indicates that this process is operative after
only a few days of food deprivation” and then “During fasting the elevated
levels of both FFA and KB exert a suppressive action on gluconeogenesis, they
maintain glucose concentration at low levels and they protect the protein
stores”. A similar conclusion is reached in the review of the subject by Tessari
et al (1996), which provides a substantial number of further references. What
many of these papers, referenced in this review by Tessan et al point out is
that there is not just one factor which is responsible for the pattern. It
depends on a balance of the level of the substrates and the balance of the
influence of the many hormones which, as shown in various discussion papers for
the Working Group are substantially changed during the administration of VLCD as
the sole source of nutrition.
It has been argued that the paper
by Halliday et al (1993) speaks about “this apparent sparing of protein is
solely due to the increased rate of protein synthesis”. This is exactly what one
would expect to see (Williamson et al, 1977; Nair et al, 1988; Crowe et al,
1989; Halliday et al, 1993). In this respect we would draw attention to the
paper by Nair et al (1988) which appears to be particularly pertinent.
There is a constant flux of amino
acids from tissue proteins, a flux that is increased during weight loss. When
glucose levels are low, but there are adequate levels of ketone bodies and FFA
available to provide for both brain and muscle metabolic needs, gluconeogenesis
decreases and free amino acids in the circulation encourage protein synthesis
producing exactly the effect that have been described by several groups and to
which attention has been directed
The main evidence advanced by
those who favour the non-ketogenic solution are the Vazquez papers. The Vazquez
et al (1995) paper is quoted as demonstrating that the cumulative nitrogen
losses are lower in the high carbohydrate groups. Unfortunately the Kjeldall
nitrogen observations must be treated with reservation (see section 3.1.2 for
discussion on this aspect). Specifically, in the Vazquez et al (1995) study, by
day 28 the subjects receiving 70g/day were in positive nitrogen balance which is
impossible during weight loss (see sections 3.2-3.6).
The Vazquez & Adibi (1992)
study has no relevance to the discussion. The ketogenic diet which they used
contains only 10g available carbohydrate per day. Since the pioneer studies of
the 1970s (e.g. McLean Baird & Howard, 1974) it has been known that at
carbohydrate levels below 30g/day, there is substantially greater protein
breakdown than above 30g. At the other extreme, they used 86g/day for their
non-ketogenic diet. Since they did not study any intermediate carbohydrate
intakes (e.g. between say 30g and 45g/day) it can not be concluded that this
would not be just as beneficial as the 86g/day.
The Vazquez also relies heavily
on leucine data. Leucine data has been criticised at various times as not being
fully representative of the protein economy. For example in the study by Bowtell
et al (1998) on the modulation of total body protein metabolism by variation in
dietary protein it appeared that leucine oxidation is very dependent on leucine
availability rather than on other factors.
This is supported by the further
study by the Bowtell group (2000) which demonstrated that the sparing effect of
glucose on leucine oxidation appeared to be dependent on a previous high protein
intake. In that particular study their low protein intake at 0.7g/kg/day (as
opposed to the high intake of 1.8g/kg/day for the high protein group) and this
low protein intake would be broadly that used in the VLCD studies. Another
observation that raises doubt about relying too heavily on leucine tracer
studies is that of Pannemans et al (1997). They used both 15N-glycine and
–[1-13C]-leucine in the same protein balance study and found that in fasting
elderly women who were consuming a 20% rather than a 10% protein diet, protein
turnover (both anabolic and catabolic) was higher as measured by glycine but
equal in both diets as measured by leucine. Furthermore, in the Halliday et al
(1993) paper which has already been quoted, further differences are high-lighted
between glycine and leucine measurements, though not in the same study.
We would therefore submit that
there is no uncontroversial evidence that there is a protein sparing effect with
the higher carbohydrate level which will ensure an absence of ketosis. With the
very substantial amount of evidence that at levels below 45g/day available
carbohydrate, there is no justification
3.9 Observations made
after the circulation of the first draft of the report to the working
group.
“1. I am
very concerned about having section 6.3 (on nitrogen balance), in the present
form and section 7.3 on the ratio between the fat mass/fat free mass ratio
being constant in the same document. If you accept section 7.3, the protein mass
is reduced by about 25% for any weight loss. This means that there can not be a
positive nitrogen balance during any weight loss period of more than the few
initial days (glycogen and water loss). Yet section 6.3 is based on the concept
of achieving positive nitrogen balance. These two concepts are
scientifically mutually exclusive. To put both concepts in the same report
without drawing attention to the scientific contradiction would in my opinion,
lead to considerable doubts about the validity of what is in most other respects
an excellent report
2. There
is clearly still a dispute in the Working Group about the question of whether
ketogenic or non-ketogenic diets are preferable. You will note that the vast
majority of the experimental and general use experience relating to safety is at
levels which would be mildly ketogenic. The Group has already accepted that in
practice VLCD at carbohydrate levels per day over 40g (perhaps even over 30g)
are safe. The other considerations leading to a higher suggested carbohydrate
level are theoretical and largely depend upon analytical techniques which are
known to be suspect. Nevertheless, I do not believe that it is necessary to
argue this further. If the working group concludes that carbohydrate below
40g/day is undesirable, but above, say 45g/day is, in practice, reasonable and
safe this will mean that those who favour a mildly ketogenic diet can continue
to use it while those who favour a non-ketogenic one can add more
carbohydrate.
3.
Section 8.4 deals with the matter of dietary fiber. It does not reach a
conclusion on content, but in the conclusion this becomes translated into
“Fiber: 10 g to max. 30g as an ingredient” I agree that it is now desirable to
define a fiber content, but believe that the what is meant by “fiber” for VLCD
use should be clear. I equally submit that only the ‘minimum’ amount per day
about 10g should be given for the following reasons:
4.
Insoluble fibres, particularly those that can chelate and those with a
high phytate content can block at least mineral absorption. The reduction in the
availability of Ca and Mg and other minerals may be dangerous. Very little work
has been done on this in relation to high fiber use with VLCD. I would prefer
the term “insoluble or soluble fibre” which would avoid this mineral
availability problem.
5. A high
content of soluble fibre (e.g. 30g/day) without other food is very likely to
produce severe diarrhoea either by the osmotic effect or by the substantial
alteration in the intestinal flora. Other recent work with which I have been
involved suggests that this is very likely to be a problem.
6.
Examination of the fiber content of current VLCD in Table 4.2 indicates
that there is virtually no information on the effects above about 10g/day
soluble fiber. The prime role of the SCOOP report is to provide
data. I believe that this recommendation of 10 – 30 g/day goes well beyond
this.
7. If the
minimum is defined as “10 g soluble fiber” it would not stop those who
want to use more from doing so.
8. If we accept the
concept that there should be a “soluble fiber content of 10g/day” this provides
broadly about 5 g ‘available carbohydrate’ (perhaps more under certain specific
conditions). If therefore we reach a conclusion that the content should be “a
minimum of 50 g/day available carbohydrate” this equals the CODEX
content but based on 45g normal carbohydrate and 10g soluble fiber. The use of
the word ‘minimum’ would mean that those who prefer more could use more.”
SECTION IV:. MEDICAL AND SCIENTIFIC JUSTIFICATION FOR
THE USE OF MODERN NUTRIENT COMPLETE FORMULA DIETS WITH ENERGY VALUE LESS THAN
800 KCALS PER DAY
The evidence
presented in this report demonstrates that the safety of formula diets does not
depend upon the energy content but on the macronutrient and micronutrient
levels. There is, therefore, no valid reason for imposing an entirely arbitrary
lower limit on products that are available to assist those who need to lose
weight. It would be scientifically irrational to expect that energy intake per
se, as opposed to the composition of the diet would affect safety. In all
humans, the daily nutrient and energy needs are made up from both stored
deposits and dietary sources. So far as energy is concerned, even a thin 60kg
‘reference woman’ has some 115,000 kcals available from her body fat
alone. This equates to enough energy to provide for her total requirement for
some 80 days.
This discussion
paper establishes beyond reasonable doubt that the overall safety of VLCD is of the same order as that of LCD in the
800-1200 kcal range. It is difficult to be more precise than this about the
relative safety of the different energy levels of the formula diets because,
whereas the VLCD have been subjected to very extensive study over several years
the number of formal studies of the safety of LCD in the range 800 – 1200kcal)
is by comparison small.
The literature examining the use by
health clinics, and the use by consumers who obtained VLCD on free sale confirms
that they can be regarded as a valuable means of weight reduction and as an
adjuvant for the maintenance of a lower weight. But no only are VLCD as good and
safe as LCD and food based diets but they have advantages in some subjects,
viz:
·
It is widely accepted that
food-based diets (even those devised by dietitians) are far fRom ideal, both in
energy content (Stordy, 1992) and micronutrients (Fisher & Lachance, 1983).
Formula diets on the other hand provide the energy, macronutrients and
micronutrients that are required, bearing in mind that the adipose tissue
contains a very substantial energy store. Formula diets have been shown to be
more effective than normal food based diets as judged by compliance during
weight reduction- Accordingly, it should be no surprise to see that a high
proportion of recent papers, even those that advise behaviour modification and
exercise, advise food replacement with a formula food. Of these current evidence
suggests that VLCD are among the most effective diets for weight reduction and
weight maintenance..
·
There is no perfect single
weight reducing method and a variety of diets to suit differing desires and
prejudices is desirable, providing such diets do not carry additional health
hazards. This is particularly valid for diets, like VLCD, which have been
extensively studied over at least 25 years and which can be shown to exert
positive health benefits (see below).
·
There is recent evidence
that the rapidity of weight loss confers additional positive health benefits
independent of the actual amount of weight which is lost, when compared with
food-based diets or higher energy level formula diets. This applies
to
a.
the management of some
cardiovascular disorders (particularly hypertension where anti-hypertensive
drugs could be withdrawn, Kreitzman & Beeson, 1996)
b.
but particularly with
non-insulin dependent diabetes mellitus (see, for example Lean et al., 1990;
Henry & Gumbiner, 1991; Wing & Greeno, 1994; Wing et al, 1994;
Hernandez-Bayo et al, 1985) in which metabolic control and lipid profile is
markedly improved by the rapid fall in weight using VLCD.
·
Moreover, meal replacements
of various types, not specifically aimed at slimmers and therefore not
restricted under current legislation, are widely available at energy values
under 150kcal. Most of these have an inadequate nutrient content both for
essential amino acids and micronutrients. These “snacks” which are readily and
freely available can be, and are, used extensively as meal replacements for
weight reducing purposes even though they can not be advised for this use. It is
therefore highly desirable to make nutritionally complete and safer alternatives
like VLCD equally readily available
·
Additionally, in some cases,
unscrupulous claims are made for protein-rich foods supplemented with various
levels of vitamin and minerals. There is currently no means by which their use
can be controlled and the risk of inadequate nutrition is clear.
·
There is a view that a
proportion of the obese are dependent on food – probably specifically fat. With
any dependence it is vital to wean the subject off their substance of dependence
as the first stage in effecting a change in behaviour This clear benefit of
formula VLCD over traditional food-based diets has proved to be a valuable
adjunct to weight maintenance in some people.
It is therefore submitted that modern
nutrient-complete formula VLCD have an important place in weight reduction and
their availability under the same regulations as other formula diets (of
800kcals and above} is fully justified
SECTION V:.
HEALTH PRECAUTIONS DURING WEIGHT CONTROL
5.1 Medical precautions for
the use of VLCD.
There is no
dispute that like many weight loss programmes VLCD should only be used as the
sole source of nutrition by those in otherwise good health, unless the dieter is
under the advice or supervision of a medical practitioner.
A list of
contraindications has been published in most examples of the current
legislation. For some physiological and pathological conditions, we submit that
the contraindication should be absolute, that is, VLCD should only be used by
those with considerable expertise in the field. For the remainder, in our
opinion the ultimate responsibility for deciding on the balance of benefit/risk
lies with the medical practitioner, who will be best able to judge the overall
needs of the individual patient. In those circumstances we submit that VLCD
should only be used with the explicit agreement of the practitioner.
We would draw
attention to the fact that some specialist out-patient clinics have used VLCD in
a number of obese patients suffering from disorders in the list of medical
contraindications. They have encountered no problems and a high success record
(Weinkove et al., 1987. Shapiro et al., 1989 Paisey et al, 1998; Miles, Cavan
& Kerr , 2000). However, it is important to stress that considerable
experience of the use of VLCD is essential for such use.
In particular the changing attitude
towards the use of VLCD in NIDDM should be noted. This condition was originally
placed by many authorities in the list of contraindications. Recent studies
(Fukuda et al 1989. Wing et al 1991; Kelley et al 1993; Wing et al 1994; Brown
et al 1996; Gumbiner et al 1996; inter alia) have shown that VLCD (probably
intermittent use, and obviously under medical supervision) has considerable
value in the management of NIDDM. The extent of these successful studies raises
questions about the validity of the report from Koffler and Kisch (1996) in just
one unit that VLCD can lead to diabetes.
Advice that any form of dieting should be used only
under the supervision of a medical practitioner also applies to those who are
receiving an established list of prescribed medications and this list is widely
quoted in current legislation. There is little dispute about the medications in
this list. Since many patients are unaware of the nature of the medication which
they are being prescribed, we believe that the sensible advice is that any patient receiving prescribed
medication should only undertake any form of dieting under the direction of
or after receiving clearance from their medical practitioner.
A list of
contraindications to any form of effective dieting is as follows:
Physiological
situations
Children and adolescents Pregnancy and
lactation
The elderly
Illnesses and disorders
Type 1 diabetes
Recent myocardial infarction
Cardiac arrhythmias
Recent stroke or serious heart
attack
Renal disease
Major psychiatric disorders or substance
abuse
Prescription
drugs
Diuretics
Antihypertensives
Insulin and oral hypoglycaemic
agents
Steroids
5.2 Medical supervision of individuals
apparently clinically healthy apart from excess weight.
It is our view
that, while medical advice may be desirable for all forms of weight loss, it is
not actually essential for those who are overweight or moderately obese though
otherwise healthy.
Indeed the question must be raised
whether medical supervision has great merit in the management of the ” otherwise
normal overweight and moderately obese”.
·
It is clear from many
comments by patients that the medical profession in general, while accepting the
problems associated with obesity, have little interest in supervising treatment
which they regard as unrewarding. The standard medical approach is still
reported as being “You need to lose weight. Here is a diet sheet. Come back when
you have lost 15 kilos”
·
Non qualified advisors with
interest in the subject are probably just as good and careful about safety
aspects (Atkinson & Kaiser 1981; Cox et al 1990; Blackburn 1993).
·
12 of the 17 “liquid protein
death” patients had been under the direct care of medical practitioners. The
evidence in the original reports suggests that the standard of care they
provided was entirely appropriate. It is just that with an inappropriate
formulation there were not early signs that could be recognised more readily by
medical practitioners. It is just not true that “if only they had been under
appropriate medical care the tragedy would have been avoided”]
Surveys referred
to in various official reports suggest that some 30% of those who use VLCD in
conditions of free-sale consult their practitioners before starting the
diet, a proportion well above that for all other forms of dieting. The
information provided in this report con6rms that there is no evidence of a
relationship between safety and the energy intake. It is the composition of the
diet which affects the safety.
W e therefore
submit that logically, all diets, including those published in the lay media
should require medical advice for use by healthy individuals or none should. It
is however suggested that attention should be directed to the fad diets and
nostrums which are widely advertised and available in the European Union with no
controls, no benefits.
The information in this discussion
paper does however support the view that for those who suffer from certain
illnesses or disorders, for those receiving defined medications, as well as
those needing to lose substantial weight by any method there should be
requirement that they seek medical advice