Author Archives: Lipotrim
Very low calorie diets in diabetes: the Bournemouth experience
Pat Miles, David Kerr
Introduction
The therapy of obese patients with poorly controlled diabetes is a complex area. Despite the best efforts of healthcare professionals and patients, therapy is too often associated with repeated failure, which can give rise to frustration and sometimes despondency. Very low calorie diets (VLCDs) have been advocated for this population group. This article looks at the process and outcomes of one VLCD programme. The results support the wider adoption of VLCDs, but there are significant resource implications which are also discussed.
The treatment of the obese individual with poorly controlled diabetes is a common and perplexing problem. Wading in with ever increasing amounts of insulin without giving thought to ameliorating the inevitable weight gain will cause desperation in the multidisciplinary team and despondency in the patient. Very lowcalorie diets (VLCDs), of <800 kcal perday, are designed to achieve substantial weight loss while preserving lean body mass and are typically associated with a 20 kg weight reduction in three months (NTFPTO, 1993). Unfortunately, regain of half to two-thirds of the initial weight loss is common within 12 months after cessation of the diet, although there may be longer term benefits in terms of a reduction in the need for medication in obese individuals with diabetes (Wing et al, 1994). Recently, Paisey et al (1998) compared VLCD with a traditional intensive dietary regimen in 30 obese (BMI>30) patients with diabetes and 19 obese controls without diabetes. After four months of VLCD, subjects were switched to a low-fat diet and continued to be seen weekly by the multidisciplinary team. Weight loss was substantial and maintained after cessation of VLCD (mean 14kg at 12 months), and 14 of the 15 patients who had chosen VLCD had normal blood glucose and fructosamine levels despite stopping all medication. For four patients with recent-onset diabetes, normalisation of blood glucose levels was sustained for 12 months.
Study aim
A pilot study was carried out to examine the effect of a VLCD programme on a group of obese (BMI30) patients with diabetes. These patients remained obese despite enormous efforts by the multidisciplinary team (including primary care). Usually, there was also poor glycaemic control. Method Between January and June 1999, 24 patients aged 29–76 years were enrolled into Lipotrim (Howard Foundation Research, Cambridge, England), a VLCD programme which gives 450 kcal per day for women and 600 kcal per day for men. For entry to the programme, each patient had to:
- Understand the programme
- Desire to take partUndertake to attend weekly individual and group sessions
- Have family support
- Be desperate or determined to lose weight.
The product was available from the hospital at a cost of £18 per week for women and £24 per week for men. The expenditure for each patient was offset against money saved by not purchasing normal food. Lipid-lowering medication was stopped on entry to the programme. Weight, blood pressure and urinary ketones were measured once weekly up to refeeding then weight and blood pressure were measured at every patient contact thereafter. Lipid levels and HbA1c were measured at the start of the programme, every month for the first six
months then at three-monthly intervals for the next six months. Patients were expected to attend the individual and group sessions at each visit (every week). In the individual sessions with the nurse, patients could discuss any problems they had encountered (Figure 1). Group sessions provided support, an opportunity to exchange experiences and preparation
for refeeding. The dietitian was involved around the time of refeeding, to reinforce product literature from the company. Most patients refed at 3–4 months, and then followed a low fat healthy eating plan. After refeeding, follow up continued weekly for the first month, then every 2–4 weeks (frequency at the patient’s discretion). However, group sessions stopped at six months into the programme.
Results
Average body mass index (BMI) was 39.5 at the start of the study.
Of the 24 patients:
- 16 were being treated with insulin
- 14 were hypertensive and were receiving appropriate medication
- 14 had dyslipidaemia and were receiving appropriate medication
- 2 were suffering from sleep apnoea requiring continuous positive airways pressure
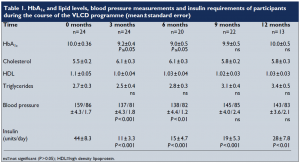
Following the introduction of VLCD, there were significant reductions in body weight (Figure 2) and BMI (Figure 3). Data on HbA1c levels, plasma lipids, blood pressure and insulin requirements of programme participants are shown in Table 1. Plasma lipid levels remained largely unchanged. Only four patients restarted lipid-lowering medication after refeeding.
Blood pressures dropped significantly within the first week, and adjustment of antihypertensive medication was necessary on a regular basis. Eleven patients stopped all antihypertensive medication. For most patients, ketone levels were moderate to high during the VLCD (indicating adherence to the programme and utilisation of fat stores). Insulin doses were decreased by two thirds on commencement of the programme, and this seemed to work well, with insulin doses continuing to decrease as weight loss proceeded. Most patients who remained on insulin were changed to nocte insulin
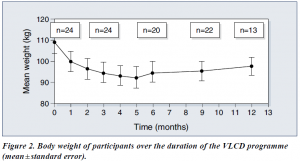
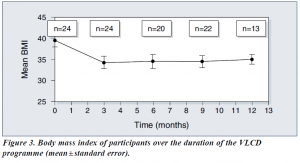
when their requirements were less than 14 units a day. Sulphonylureas were also halved or stopped on commencement of the programme. Only 13 patients completed follow up for the 12 months of the programme. The three case histories (see page 111) provide further detail about some of the patients in the programme.
Discussion
Benefits of VLCD
VLCDs can be an effective method of reducing weight, improving glycaemic control
— at least in the short term — and reducing the need for concomitant medication in
obese people with diabetes. They can also allow individuals to gain insights into the potential benefit of weight reduction and to learn about the relationship between food and obesity. When asked why this diet had worked while all others had failed, our patients said that it was easier to have no food at all, than to try to make choices from food offered, particularly on social occasions. Also the rapid weight loss experienced on the programme was positive reinforcement, together with the feeling of ‘wellbeing’ experienced as a consequence of ketosis (Burley et al, 1992).
Some considerations
It is well known, however, that helping someone to maintain weight loss is often the most difficult and disappointing task (Wing, 1995). In addition, the process is very time consuming for any healthcare professional involved. This pilot project to examine the effectiveness of VLCDs involved seeing 24 patients every week for 3–4 months, then at least monthly for the following nine months. We have only touched the ‘tip of the iceberg’ in our clinic population. If this service were offered to all of our obese patients (at least 60% of the total), a 50% uptake would involve 2250 patients who would require 11 whole time equivalent healthcare professionals just to provide weekly visits! In practice, this would be unrealistic and unlikely to attract funding, though one could argue that treating the root cause of the problem is far better than attempting to treat the effects. Putting VLCD into practice In many areas, primary care is offering Lipotrim to its obese patients. If the expertise of practice nurses and community dietitians in using this product could be built up, and the diabetes team was available for advice on medication changes for people with
diabetes, then it could be possible to offer this service more widely and cost effectively.
However, because of the additional risks of hypoglycaemia and ketoacidosis in patients with type 1 diabetes, we feel that they should only be offered the programme under the supervision of an experienced diabetes team, and then only if the patient is able to self-adjust insulin appropriately and understands the risks.
Conclusion
This study advocates the use of VLCDs for reducing weight and improving glycaemic control in obese people with type 2 diabetes (as well as carefully selected people with type 1 diabetes under close supervision). VLCDs can also reduce the need for concomitant medication. While on a VLCD, individuals can become empowered through their increased awareness and knowledge of their diabetes and the positive feedback provided by the rapid weight loss. It is likely that lack of time would limit the widespread adoption of the VLCD service used in this pilot study. However, the potential benefits of VLCD make it worthwhile to try to produce a costeffective service, perhaps by increased primary care involvement.
PDF Version: bournmouth-miles-kerr
Gratis Journal of Biomedical Sciences
Weight Loss Achieved by Overweight and Obese Subjects Entering the
Lipotrim® Weight Loss Programme Monitored by Pharmacists in England
Thurnham David 11*, Beeson Valerie2 and Kreitzman Stephen N2
1Northern IrelandCentrefor Food&Health,Schoolof BiomedicalSciences, UniversityofUlster,ColeraineBT521SA, UK
2Howard Foundation Research Ltd, Downing Park, Station Road, Swaffham Bulbeck CB25 ONW, UK
Received: April 21, 2015; Accepted: April 24, 2015; Published: April 27, 2015
Abstract
The objective of this report was to assess the results of a weight-loss programme managed by pharmacists since obesity and type-2 diabetes are serious problems in the UK. We evaluated the service provided by pharmacists in the UK to manage and continuously monitor a very low energy diet (VLED) program based on Lipotrim® for overweight and obese people who wished to lose weight. Between 2008 to 2013, 57 (-3%) of 2000+ pharmacies offering the service elected to utilise online tracker software instead of paper records. Extrapolation of the subject numbers from this subset to the full population presenting to participating pharmacies for weight management yields an estimate of more than 300,000 people. 8724 overweight people voluntarily enquired about the weight loss program at the 57 pharmacies. Approximately 50% of these people completed at least two full weeks and their information was analysed in this report. Of the 50% who completed two weeks, 30% (1077 women, 241 men), displayed a period of linear decline in weight and at a mean duration of —60 days, mean weight loss in women was 12 kg (-12.6% initial weight) and in men was 16.5 kg (-13.8%). The remaining 70% (2487 women, 540 men) lost 8.0 and 11.5 kg over 104 and 122 days respectively. In conclusion, weight losses in those people who persisted in the program will have a public health benefit and potentially reduce their risk of co-morbidities such as diabetes. Pharmacists in the UK are ideally placed to provide and monitor weight loss programs for overweight people.
Keywords: Obesity; VLED; Weight loss; Pharmacies; Body mass index
Abbreviations: VLED: Very low energy diet; BMI: Body Mass Index
Introduction
Obesity is closely associated with diabetes, high blood pressure, joint pain and deterioration, stroke, some cancers and heart disease [1,2] and the prob¬lems are of increasing concern in developed [3,4] and developing [5] countries. Obesity is assessed using the body mass index (BMI, weight/height squared, kg/m2). Values greater than 25 are associated with a greater risk of diabetes (specifically type-2 diabetes), cardiovascular
disease and cancer and persons with BMIs >40 (class III obesity) have substantially increased rates of mortality [3]. Currently persons with a BMI between 35 and 40 kg/m2 and already having a significant
disease such as type-2 diabetes can be considered for bariatric surgery. However, bariatric surgery is an expensive procedure and not without its own problems.
Complication rates are high and can be very serious [6].
A reduction in weight by overweight people has been shown to reduce the risk of diabetes [7,8]. The natural
way to lose weight is by reducing food, or specifically calorie, intake; that is dieting and/or an increase in calorie expenditure i.e. physical activity. Furthermore dieting is relatively cheap and does not carry any surgical risks. Unfortunately, successful dieting is notoriously difficult as indicated by the number and variety of dieting methods available to the general public.
Hospital studies have shown that successful weight loss can be achieved using structured weight loss programmes using very low energy diets (VLED) [9] and that long term weight-loss maintenance is significantly
greater than that following successful hypo-energetic diets in both men and women at 4 to 5 years of follow-up [10]. Although hospital studies of the effects of VLEDs on overweight people have been shown to be a highly efficacious method of reducing body weight [9], being overweight or obese is usually not a clinical condition and hospital treatment using VLEDs is inappropriate and rarely available. Nevertheless, successful dieting requires assistance by family members or professionals or both as well as self-control.
In this paper we describe an evaluation of a service provided by English pharmacists in assisting overweight and obese people to lose weight using structured weight-loss programme based on a product known as Lipotrim®. We report weight losses achieved by two groups of these subjects; those who stick more rigidly to the weight loss plan and those whose dietary compliance is more erratic. We show that successful weight loss by both groups was achieved.
Materials and Methods
Data collection
From March 2001 an expanding list of pharmacists, currently over 2000, have offered a professional service to assist in obesity prevention and treatment where overweight people wish to lose weight. Trained pharmacists supervise and monitor dieters using the Lipotrim® formula foods and, importantly, they can also offer a follow-up weight maintenance program and supervision but that is not the subject of this report. Lipotrim ® is sold through pharmacies throughout the United Kingdom and data on weight, height, age and sex are recorded by the pharmacists for those people who voluntarily enrol in the programme. We emphasize, participation in the weight loss programme by members of the public is entirely voluntary i.e., they continue for as long or as little as they wish. Participants buy Lipotrim® products from the pharmacists and attend weekly for professional monitoring; recording of weight, reporting of any changes in their medical condition and obtaining enough formula for a subsequent week. At the time of the assessment reported in this paper, 57 (~3%) of the pharmacies’ records were kepton-line using Lipotrim® patient tracker secure software
(Backup Data Ltd 15 Sable Close, Cambridge, CB1 9YX). These data are used by the pharmacists to monitor a subject’s progress and the on-line service permits the suppliers to assess the collective success of the pharmacy’s service in weight management.
Height and weight were recorded by the individual pharmacists using equipment supplied at no cost by Howard Foundation Research Ltd. Weights were recorded using precision scales (UC-321PL, A & D Medical, 24-26 Blacklands Way, Abingdon Business Park, Abingdon, Oxfordshire OX14 1DY). Height was measured by a Seca 206 Roll up Measuring Tape (Seca, 40 Barn Street, Birmingham B5 5QB). Names and addresses, recorded at the pharmacy as part of the pharmacy’s records, were not available beyond the specific pharmacy, but subjects were allocated a unique number so a subject’s weight loss data could be included in the overall outcome assessments.
All anonymized data was made available online to The Howard Foundation Research Ltd. Subjects who did not complete 2 full weeks were removed from the analysis. This paper will report only the data collected on the tracker database from English pharmacies over the six years from March 2008 to May 2013. These data were collected from 3564 female and 781 male weight loss records 97.5% of which were accumulated by 57 pharmacies who submitted records for four or more subjects on line between 2008 and 2013.
Dietary regimen
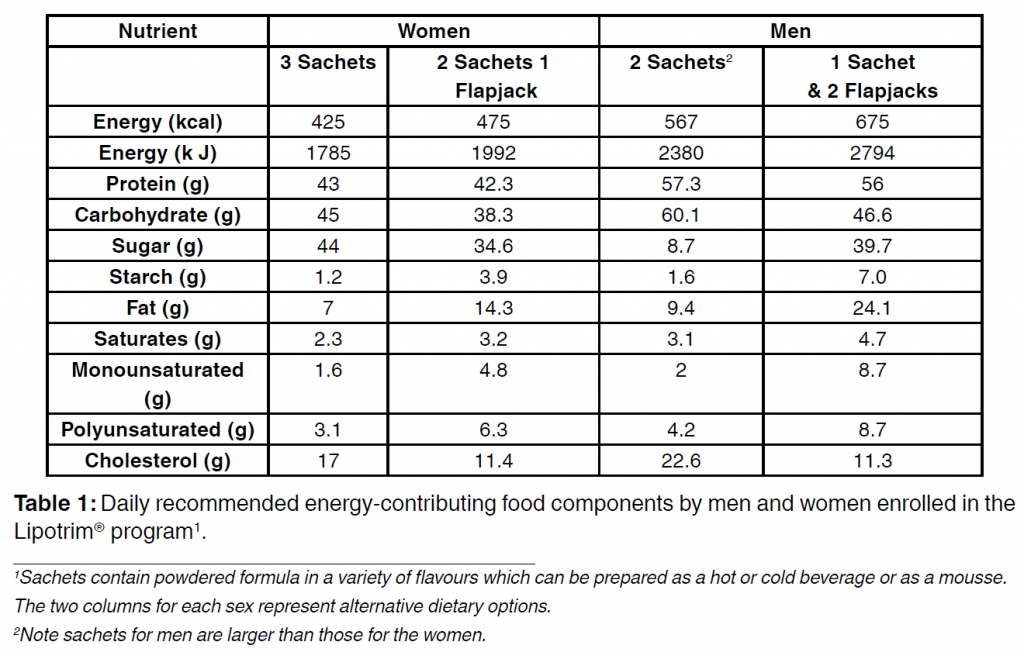
Lipotrim® is a very low energy diet (VLED) and the components contributing to the energy intake are shown in Table 1. A daily serving contains all the required essential amino acids, essential fatty acids, trace elements, vitamins and minerals in amounts which
meet 100% of the recommended daily allowance. Instructions on the use of the product are provided by the pharmacy and also accompany the packaging. The products are intended as a total food replacement and for full compliance, additional food is not permitted. The product is designed to reduce energy intake to the minimum consistent with complete nutrition and is provided as sachets of different flavoured powders and as flapjacks with two flavours. Female participants are instructed to consume 3 sachets a day or two sachets and a flapjack and for men, two larger sachets per day or 1 larger sachet and 2 flapjacks. Constituents of the sachets for men and women are identical in composition but men, who have higher nutritional requirements because of a higher metabolic rate due to a greater muscle mass, have more of the diet (Table 1) but the flapjacks are the same. Three sachets for a woman provide 1785 kJ (425 kcal) and two sachets for a man provide 2380 kJ (567 kcal). If participants adopt the flapjack option, total daily energy consumed is 1991 and 2381 kjoules (474 and 675 kcal) for women and men respectively. All the products are gluten free and suitable for vegetarians. Sachets can be prepared as a drink (hot or cold) or as a mousse and guidance is given to ensure that subjects using Lipotrim® as a total food replacement consume at least 2 L of water per day. The Lipotrim® program comprises three distinct phases to ensure that the subjects achieve and maintain weight loss: strict weight loss, transition and maintenance. Only weight loss results are presented here.
Ethical considerations and participation in
the weight-loss programme
This paper is an evaluation of the program provided by pharmacies and as such does not require ethical approval in the UK [11]. The subjects voluntarily entered the weight-loss programme and gave their informed consent to the use of their anthropometric and medical history results by signing the following statement.
“I declare that the above answers are true, that I have not omitted any material information and that I authorise the release of the findings of this questionnaire to Howard Foundation Research Ltd”. Healthy overweight people, i.e. those with no medically-treatable condition that would be contraindicated on a VLED, such as during pregnancy or immediately following major surgery, stroke or heart attack. or on medication with a narrow safety spectrum, such as warfarin or lithium, whose absorption rate can be altered leading to inappropriate blood levels, can immediately enter the program after signing the above statement. For subjects with type-2 diabetes, the pharmacist must also obtain the GP’s agreement to suspend diabetic medication. The weight loss will result in a rapid normalisation of blood sugar concentrations and continued medication can cause problems. Patients on mediation with a narrow safety spectrum require
medical cooperation to closely monitor blood levels.
Statistics and calculations
Statistics were done using SPSS version 19. Most data were normally distributed and are therefore shown as means and standard deviations. The only exception
was the days duration of dieting which was positively skewed. Differences in anthropometric data between the sexes was determined by independent ‘t’ tests.
Bivariate analyses and multiple linear regression was used to investigate relationships between the anthropometric data and weight loss. To identify fully-compliant dieters and calculate the kjoules (kcal) deficit per day, weights were plotted against days on the program for each individual. Fully-compliant dieters were identified when the linear correlation of at least 5 successive weekly differences in body weights plotted against days had an r2 greater than 0.9. For these subjects the computer algorithm calculated the weight loss in g/day for the linear region of the diet plot after the first month of dieting. During this period, weight lost is predominantly fat at 37800 kjoules (9000 kcal)/kg. However, this weight loss (energy depletion) occurs in the face of the energy intake from the VLED, therefore, the total daily energy utilisation (i.e. deficit) during the linear period is calculated as follows.
Estimated energy deficit
(kcal)/day = (weight loss × 9 kcal/g) + VLED
Where: weight loss is in g/day from the regression
equation
VLED is 425 and 567 kcal in Lipotrim® for women and
men respectively
kjoules = kcal × 4.2
Results
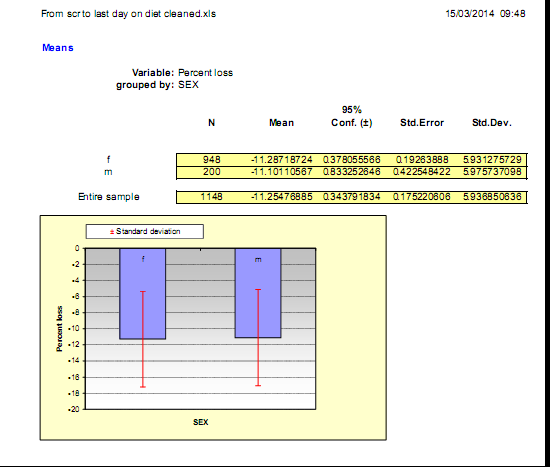
Anthropometric and limited demographic information was available from the 4344 subjects (3563 women and 781 men) who voluntarily started the Lipotrim® weight loss program and continued for variable lengths of time in excess of two weeks. These data represent approximately 50 % of subjects registering on the program at a subset of 57 pharmacies, since entries for subjects who did not complete two full weeks were removed from the analysis. The subjects not included were not necessarily dieting failures. Some subjects elected to try alternative methods of weight loss, some decided to postpone proceeding for personal reasons or, after learning what was involved for participation, decided the diet was not for them. The valid data were subdivided into two groups, those whose records
showed a period of linear decline in weight with time (compliant dieters, 1077 women and 241 men) and those whose weights fluctuated over the period of enrolment (erratic dieters, 2486 women and 540 men).
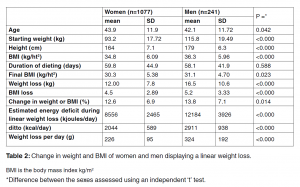
Table 2 shows the weight loss data for the compliant dieters. Mean ages of the women were slightly greater than those of the men (P=0.042) and the age range stretched from 18 years to 74 and to 75 years in women in men respectively. Starting weights and BMIs of the men were both significantly higher than those of the women (P<0.000). There was no difference in the duration on the weight loss program in the two sexes (p=0.588). The mean weight loss in the women (12 kg) was less than that in the men (16.5 kg; P<0.000) and mean weight loss as a percentage of initial weight was 12.6% in the women and slightly greater (13.8%, P=0.014) in the men. The mean weight loss over the total period of dieting was 226 or 324 g/day in men and women respectively. Approximately 16% (n=209) of these dieters lost 20% or more of their initial weight and the maximum weight lost by any dieter in the program was 55.5 and 84.6 kg in the women and men respectively.
In the compliant dieters, the mean estimated energy deficits per day during the linear phase of the diet plan were 8585 and 12,262 kjoules (2044 and 2911 kcal) in women and men respectively. To calculate the mean daily weight loss from the energy deficit during the linear phase of dieting, energy intakes from the VLED were first subtracted (1619, 2344 kcal) and these values divided by 9 (energy value of fat) to give 180 and 260 g/day in women and men respectively.
That is the mean energy deficit per 100 g weight loss was approximately the same; 3776 and 3788 kjoules (899 and 902 kcal) in women and men respectively.
Although the mean energy deficits were approximately the same as the accepted values for the energy required for maintenance of weight [12] the standard deviations attached to these values are large for both women and men and indicate considerable variability in the estimated energy deficit needed for weight loss.
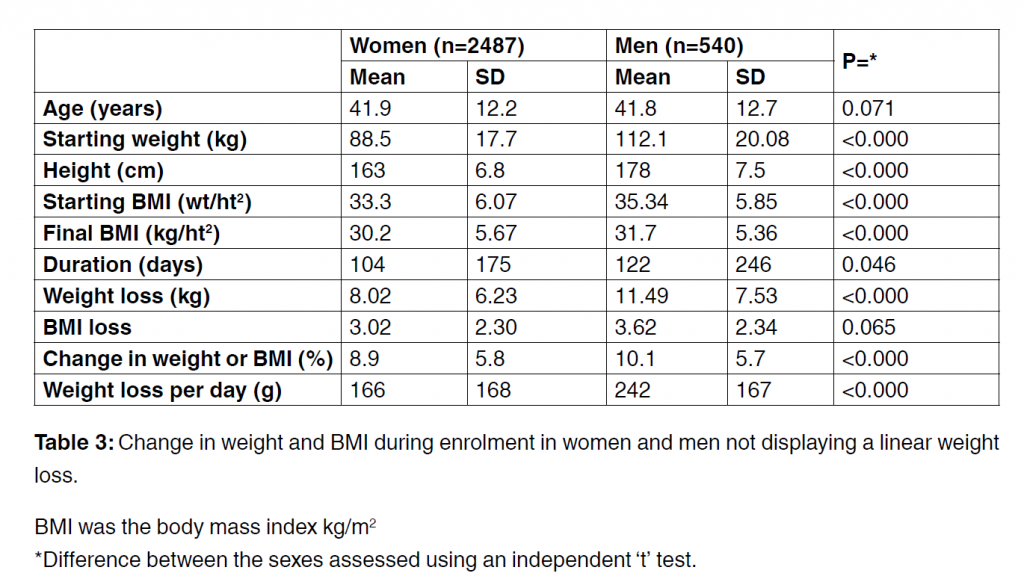
Table 3 shows weight loss data in those with a more erratic weight decline indicating somewhat less than strict adherence to the VLED protocol. There were no major differences in ages or anthropometric details between these dieters and those displaying linear weight loss. Mean dieting duration times however was almost twice as long in the erratic dieters; 104 and 122 days
in women and men respectively. The mean weight loss over this time was 8 kg in the women and 12.5 kg in the men, a drop of 9 and 10% respectively of starting weights. Only 5% (n=158) lost more than 20% of their initial weight but the maximum weight lost by any dieter was 124 and 66.4 kg in the women and men respectively. In the more compliant dieters we explored the relationships
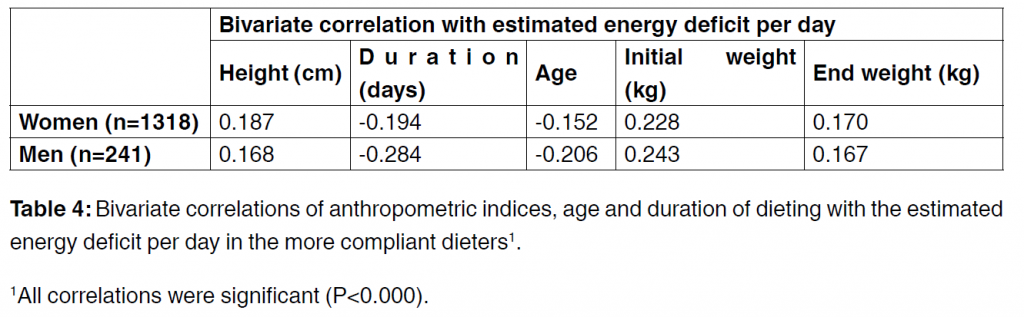
between the anthropometric factors and the daily estimated energy deficits (Table 4). Height and initial and end weights were positively related to the calories lost per day while age and dietary duration were negatively related. Multiple linear regression of the data showed that these variable explained 31% of the variance in men and 24% in the women. The principal factors in both sexes were approximately equal contributions from an inverse relationship with the duration of dieting and a positive relation with initial weight. Together these variables explained 20% and 12% of the variance in the men and women respectively.
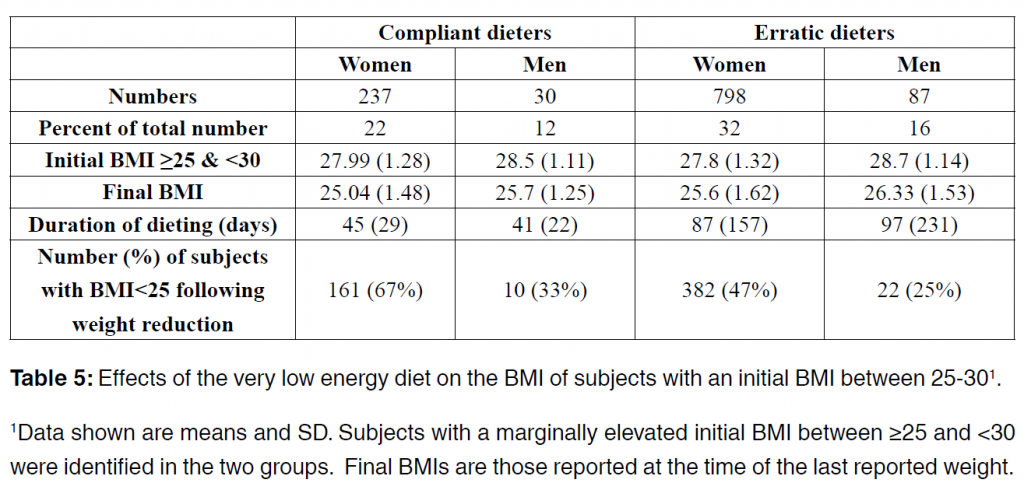
In both dieting groups, the final mean BMI fell from around 34-35 to 30-31. It was of interest to know how subjects with less severe obesity responded to the diet. We identified overweight, but not yet
obese subjects with BMIs between 25 and 30 and found in both groups the effect of the diet was to reduce BMIs to a mean value of approximately 25 (Table 5). That is approximately half of the subjects in this specific group achieved the healthy weight range.
Discussion
This study provides documentation of the successful weight losses in overweight people who voluntarily chose to take part in a weight-loss program managed by pharmacists. They had not incurred the risks and costs of bariatric surgery and did not have the assistance of a dedicated hospital VLED program if one was available. The data suggest that close adherence to the Lipotrim® diet by dieters in their own homes reduced mean weights
in women and men by 12 and 16.5 kg respectively; that is reductions of 12.6% and 13.8% of starting weights in approximately two months. Even women and men who did not adhere strictly to the recommended program and consequently did not achieve a linear weight loss, were nevertheless able to reduce their weights by 8 and 12.5 kg. These reductions represented 9 and 10%, respectively
of their starting weights but the time taken was 70-100% longer than that in the compliant dieters.
At the time of this assessment 8724 overweight people registered for the weight loss program at 57 of 2000+ pharmacies, which facilitated this evaluation of the program. Extrapolation of the subject numbers from this subset to the full population presenting to participating pharmacies for weight management yields an estimate of over 300,000 people. From discussions with participating
pharmacists we can reliably assume that at least half this number will have achieved weight loss in excess of 9-10% of their initial body weights in two to four months.
There is a close association of overweight with a higher risk of diabetes [6] and weight loss has been repeatedly shown to reduce the prevalence of diabetes and lower cardio-metabolic risk [9,13]. In a 10 year community study of weight gain and loss in 1929 overweight people, there were 251 incident cases of diabetes.
Workers found that relative to those with stable weight, each kg of weight loss annually was associated with a 33% lower risk of diabetes in the subsequent 10 years whereas one kg of weight gain was associated with a 49% increased risk of developing diabetes [7]. Likewise, workers studying weight, diabetes prevalence and mortality over 30 years from 1980 to 2010 in Cuba during an economic crisis and a subsequent recovery, found that a 5.5kg weight loss over the whole population during the crisis was associated with rapid declines in diabetes and heart disease which rebounded
once economic conditions improved [8]. Thus weight loss in the community can have long-term beneficial effects on health and it is important that the progression to obesity is prevented. These and other studies show that the adverse health consequence from excess weight can begin long before weight reaches a BMI of 30, the so called ‘obesity boundary’ [14,15].
This is particularly true for certain ethnic populations, especially South Asians who have the same risk of diabetes at BMI 24 as white populations at BMI 30 [16].
For overweight patients, and especially those at higher levels of obesity, losing weight can be extremely difficult and standard approaches to weight loss have been less effective than VLEDs [17]. Many obese patients fail because they are attempting to control addictive behaviour while continuing to use the ‘substance of abuse’ – food. This approach does not work for alcohol, tobacco or drugs and it rarely works for food [18]. For seriously overweight people, the most effective treatment is to totally stop the substance of abuse, which is why a total food replacement program is much more effective
than trying to cut down on conventional food intake [19].
From a physiological point of view the human body does not require food as such but essential nutrients, specific chemical compounds of which people require a sufficient supply to stay healthy together with a source of fibre to provide bulk. These nutrients are normally supplied in the diet but as there is no single food that exactly matches all human nutritional needs, it is necessary ordinarily to obtain them from a diverse range of foods. Obtaining the required complement of nutrients from common foods requires the consumption of many more calories than is consistent with rapid and substantial weight loss. The advantage of a total food replacement program is that nutrition is provided by an engineered formula that is nutritionally complete, allowing the dieter to remove the variable components (i.e., food) from his or her life while weight is lost and the medical consequences of the excess weight are relieved. The total food replacement regime is arguably the only non-surgical means by which those who consume excessive amounts of food may avoid the stimulus that perpetuates their weight problem. The most salient fact that weight loss in overweight or obese people achieves is a reduced risk of diabetes or remission of established diabetes.
A limitation of this report is that we only have weight loss records for 50% of those subjects who initially enquired about the Lipotrim® program and subsequently dieted with Lipotrim®. Participation in the program was entirely voluntary and does require firm commitment to the dietary regime. Prospective dieters are required to view, and sign that they have viewed, a DVD that fully details the program, its strict requirements and potential side effects. When the DVD is loaned to the potential dieter, the record is retained on the computer, but if the person does not undertake the program,
there is no further data. Not all people are willing to undertake such a strict program, but it is usually not possible to determine the reasons why an individual declined the program. In addition because of the confidential nature of the program, no medical records were available to us beyond the initial medical questionnaire, so a further limitation of this report was the lack of evidence supporting the long term benefit to diabetic patients. Only two weight loss methods, bariatric surgery and VLED, reliably provide sufficient weight loss rapidly enough to enable long term glycemic control in diabetic patients [9] however since only diabetic patients whose doctor authorized suspension of medication were permitted to diet we can reasonably assume that restarting medication became unnecessary
in most, if not all the type 2 diabetic patients Any person receiving treatment for diabetes would not have started the VLED until the pharmacist had discussed their treatment with their general ractitioner and their treatment modified. It has been known for almost 40 years that excessive blood glucose concentrations fall in subjects on a VLED [20] and this was clearly shown by Henry and co-workers in obese subjects with type-2 diabetes whose blood glucose concentrations fell by 50% after 10 days on a VLED and there were further reductions on day 40 [9]. It is important therefore that overweight person with diabetes do not start a VLED program without first withdrawing blood glucose-reducing medication.
The information in this report was from subjects who were not part of a research program so they were not under any obligation to continue with the pharmacist. The last recorded weights illustrate that the more compliant dieters achieved appreciable weight loss in approximately two months on the VLED. Henry and colleagues achieved a mean weight loss of 10.5 kg (SD 0.4) after 40 days in 30 obese subjects who consumed 330 kcals/day [9]. The weight loss achieved by the subjects enrolled in the pharmacies for a mean duration of 60 days and who had slightly higher energy intakes, was 12 and 16.5 kg in the women and men respectively. That is weight loss by the pharmacy subjects was comparable with the more controlled hospital study of Henry and colleagues [9].
The effect of VLEDs on overweight people is a highly efficacious method of reducing body weight since the calories supplied are insufficient in all adults to meet even basal metabolic needs, regardless of size or activity.
The body therefore has to draw on energy reserves to supply the needed calories. The total mean weight loss per day by the more compliant dieters was 226 and 324 g for the women and men respectively. However, during the linear phase of dieting when body fat is the principal tissue being consumed, weight loss per day was 180 and 260 g/day in women and men respectively.
The average energy deficit needed to produce weight loss during the linear phase was approximately 4720 kjoules (1124 kcal) per 100 g weight loss in both women and men. It follows that if dieters should eat more than the recommended diet during the linear phase they will lose less weight and vice versa. However, deviations from the programme would lead to a loss of linearity and subjects would not have been included in the linear group. Nevertheless, small deviations from the recommended diet programme as well as life-style and genetic factors may explain the wide standard deviations of the energy deficit needed to produce this weight loss. That is the energy deficits to produce weight loss in some people are much smaller than in others. It can be speculated that if people have only a small energy deficit when consuming the recommended VLED intake then it follows that a smaller number of calories may only be needed to regain that weight and vice versa. That is these data may provide some guidance for the pharmacist on the number of calories needed by their patients during weight maintenance when dieting has finished and they request advice to maintain their lower weight. Weight maintenance however was not a component of these studies.
Conclusion
Pharmacists in England who utilised the Lipotrim® VLED and also recorded the data on-line with the Lipotrim ® Patient Tracker software, were approached by 8724 overweight people between March 2008 and May 2013. Fifty percent of these subjects (n=4344) voluntarily participated in the programme and successfully completed at least 2 weeks dieting. Of these, 30% (n=1318) achieved linear declines in weight over a mean duration of 60 days and the weight loss evidence suggests they were more compliant with the dietary program than the remaining 70% (n=3026). These subjects
lost weight but dieted for almost twice as long. The data show that pharmacists supervising the Lipotrim ® VLED in free-living, compliant overweight men and women were able to assist their subjects to lose mean weights of 12 kg in women and 16.5 kg in men.
In the less-compliant subjects, mean weight losses of 8 and 11.5 kg in women and men respectively were obtained. From a public health viewpoint, overweight subjects
who can adhere to a VLED can achieve sufficient weight loss to reduce their risk of type 2 diabetes and cardiovascular disease. Pharmacists are ideally placed to supervise a VLED program for the general public.
Acknowledgements
We acknowledge the very great help and assistance from pharmacists in obtaining these data up throughout England.
Authorship Contributions
SNK and VB provided the database for analysis and DIT prepared the initial draft of the paper. All authors approved the final draft. None of the authors were involved in the data collection which was done by the individual pharmacies.
Conflicts of Interest
SNK and VB are directors of Howard Foundation Research Ltd. DIT is a consultant for Howard Foundation Holdings Ltd.
References
1. Bray GA (2004) Medical consequences of obesity. J Clin Endocrinol Metab 89: 2583-2589.
2. Bhaskaran K, Douglas I, Forbes H, Dos-Santos- Silva I, Leon DA, et al. (2014) Body-mass index and risk of 22 specific cancers: a population-based cohort study of 5.24 million UK adults. Lancet 384: 755-765.
3. Kitahara CM, Flint AJ, Berrington de GA, Bernstein L, Brotzman M, et al. (2014) Association between Class III Obesity (BMI of 40-59 kg/m2) and Mortality: A Pooled Analysis of 20 Prospective
Studies. PLoS Med 11: e1001673.
4. Wang YC, McPherson K, Marsh T, Gortmaker SL,Brown M (2011) Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 378: 815-825.
5. Singh PN, Arthur KN, Orlich M, James W, Purty A, et al. (2014) Global epidemiology of obesity, vegetarian dietary patterns, and noncommunicable disease in Asian Indians. The American Journal of Clinical Nutrition 100: 359S-364S.
6. Andrews RC, Chen MZ, Longue J. Bariatric surgery for type 2 diabetes always produces a good outcome. Practical Diabetes 31: 376-380.
7. Resnick HE, Valsania P, Halter JB, Lin X (2000) Relation of weight gain and weight loss on subsequent diabetes risk in overweight adults. J Epidemiol Community Health 54: 596-602.
8. Franco M, Bilal U, Ordunez P, Benet M, Morejón A, et al. (2013) Population-wide weight loss and regain in relation to diabetes burden and cardiovascular mortality in Cuba 1980-2010: repeated
cross sectional surveys and ecological comparison of secular trends. BMJ 346: f1515.
9. Henry RR, Scheaffer L, Olefsky JM (1985) Glycemic effects of intensive caloric restriction and isocaloric refeeding in noninsulin-dependent diabetes mellitus. J Clin Endocrinol Metab 61: 917-
925.
10. Anderson JW, Konz EC, Frederich RC, Wood CL (2001) Long-term weight-loss maintenance: a meta-analysis of US studies. Am J Clin Nutr 74: 579-584.
11. www.hra.nhs.uk/documents/2013/09/defining-research.pdf
12. Department of Health (2013) Dietary Reference Values for Food Energy and Nutrients for the United Kingdom. Report on Health and Social Subjects, No. 41. London: HMSO.
13. Kelley DE, Wing R, Buonocore C, Sturis J, Polonsky K, et al. (1993) Relative effects of calorie restriction and weight loss in noninsulin-dependent diabetes in women. Am J Epidemiol 132: 501-513.
16. Chiu M, Austin PC, Manuel DG, Shah BR, Tu JV (2011) Deriving ethnic-specific BMI cutoff points for assessing diabetes risk. Diabetes Care 34: 1741-1748.
17. Heymsfield SB, Harp JB, Reitman ML, Beetsch JW, Schoeller DA, et al. (2007) Why do obese patients not lose more weight when treated with low-calorie diets? A mechanistic perspective. Am
J Clin Nutr 85: 346-354.
18. Volkow ND, Wise RA (2005) How can drug addiction help us understand obesity? Nat Neurosci 8: 555-560.
19. Martin CK, O’Neil PM, Pawlow L (2006) Changes in food cravings during low-calorie and very-low-calorie diets. Obesity (Silver Spring) 14: 115-121.
20. Bistrian BR, Blackburn GL, Flatt JP, Sizer J, Scrimshaw NS, et al. (1976) Nitrogen metabolism and insulin requirements in obese diabetic adults on a protein-sparing modified fast. Diabetes
25: 494-504.
*Correspondence: David Thurnham, Northern Ire¬land Centre for Food & Health, School of Biomedical Sci¬ences, University of Ulster, Coleraine BT52 ISA, UK, Tel/ Fax +441223811668; E-mail: di.thurnham@ulster.ac.uk
PDF version: 24-77-3-PB (1)
Treating obesity is easy – just eat less (so the saying goes)
Assuring there will be a ‘tomorrow’s pharmacist’
Vending machines for prescription drugs are already here. How much longer will you be here?If you intend to be a pharmacist of tomorrow, you need to start acting today. Delivering a professional weight management service is a good place to start
By Dr Stephen Kreitzman Ph.D, RNutr and Valerie Beeson, of Howard Foundation Research
THE ROYAL PHARMACEUTICAL SOCIETY has set out best practice standards for pharmacies delivering public health services in England and Wales. The ‘Professional standards for public health practice for pharmacy’ were created in partnership with the Department of Health, Royal Society for Public Health and Faculty of Public Health, and focus strongly on backing up services with data. They call on pharmacists to ensure their public health offering is evidence-based, tailoring it to local needs wherever possible, and to gather data that proves the value of services
Of all the important services being offered in pharmacy, it could be argued that weight management is the most valuable and documentable. It is valuable because controlling weight prevents and can even treat type 2 diabetes, high blood pressure, depression, sleep apnoea, poor fertility and a host of other health issues that are prevalent in the community. It can even impact on services such as smoking cessation, since the possibility of weight gain is often a reason for failure to stop smoking.
A weight management service is readily documentable, since tracker software is available that will instantly provide evidence for weight loss achievements and medical benefits from the weight loss. If you can’t produce data, you have no proof of your pharmacy’s accomplishments.
The not-yet-obese
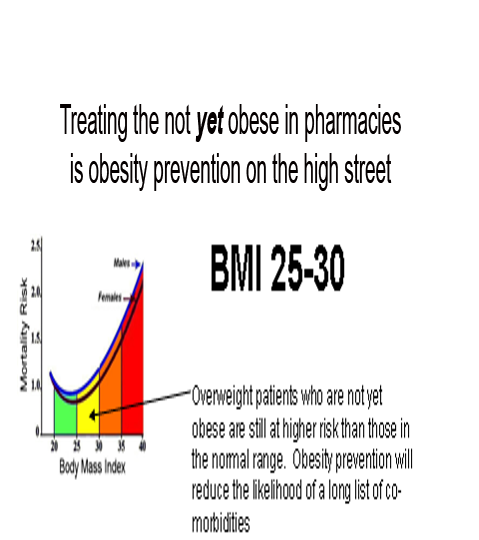
Treating overweight, but not-yet-obese, people in pharmacy, is obesity prevention on the high street. There are over 30 million overweight and obese people in the United Kingdom. Since no one ever became obese without first being overweight, it is important to provide real help to people at this stage. It is much less problematic to help people who do not have a massive amount of weight to lose and who also do not yet have some of the serious medical consequences associated with excess weight.
Pharmacy has become the prime location for weight management in the UK and Ireland. With the NHS ‘Call to Action’, pharmacy professional bodies are urging pharmacists to make their voices heard and shout about the good they do in improving people’s health.
Helping people lose weight is not just about making them feel good but is also about preventing major long-term health problems, such as type 2 diabetes. A recent article in GP magazine reported a staggering seven-fold rise in insulin use in type 2 diabetes over a nine-year period. An effective pharmacy weight management service could have an enormous and immediate benefit.
But it seems that it’s not just the NHS that needs to hear what pharmacy has to say. The public do, too. North London LPC was inundated with enquiries about a newsletter it had produced raising awareness of pharmacy services in the area.
Promote your service
So what does that mean to you as a pharmacist with a team already offering an established weight management service? Promote your service far and wide and show the public and the NHS what you’ve been doing to improve the health of the nation.
Fin McCaul, for example, is first and foremost a community pharmacist practising in Manchester. He is also the chairman of the Independent Pharmacy Federation and works for Bury CCG one day a week as its long-term conditions lead.
Fin’s passion for independent pharmacy is second only to helping patients lose weight and stop smoking. With an average of 100 quits per year and well over 1,000 patients helped through the weight loss service in his pharmacy, there is nobody better placed to talk about the opportunities and challenges for pharmacy now that public health commissioning has moved into the care of local authorities.
Delegation, motivation and marketing skills and advice for pharmacists and their team are just some of the benefits from his stop smoking/weight loss clinics. At the 2013 Pharmacy Show Mr McCaul organised a series of patient services workshops delivered by pharmacists who were successfully running weight services in their local community and wanted to share their knowledge and expertise. At the March 2014 Independent Pharmacy Federation conference, Fin again provided the opportunity for training in critical pharmacy services and the weight management clinic run by author Valerie Beeson was well attended and appreciated.
A giant change in practice
NHS England’s education arm has launched new standards for pharmacists delivering patient consultations, which have been hailed as a “giant change” in pharmacy practice. Health Education England (HEE) called on pharmacists to ensure they were educating patients, building a relationship with them and respecting their individual needs when conducting consultations.
The Westminster Food and Nutrition Forum seminar, held in London in February, kicked off with the staggering statistic that more than half of the UK population could be obese before 2050. This could create costs of £50 billion a year to the NHS, warned speakers, who included representatives from NHS England, Public Health England, NICE, the Department of Health, CCGs and the nutrition sector.
The speakers agreed that primary care is the key battleground for tackling the issue. But with GPs and pharmacists at the frontline of delivering public health services, who is better placed to keep the nation’s waistline under control? It is clearly pharmacy.
There was no doubt that pharmacy should offer obesity services. Ash Soni, pharmacist and vice chair of the RPS English Pharmacy Board argued that most overweight people did not feel unwell so would usually fail to see the point of visiting their GP. Mr Soni believed using a medical model was the wrong starting point. Most people visited pharmacies for multiple reasons, which presented an “ideal opportunity.”
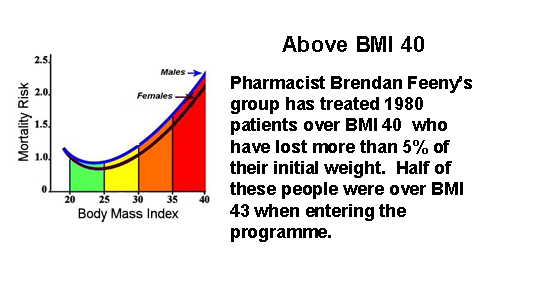
Pharmacy is an excellent provider of weight services for the community. Many overweight people in the BMI 25-30 range take advantage of pharmacy weight loss programmes, recognising that they really work and feeling confident that they are being monitored by healthcare professionals. Pharmacists’ expertise in weight management, however, has proven extremely valuable for the treatment of obese and even morbidly obese people. This is a group who could have qualified for bariatric surgery at great expense and risk.
Effective weight loss absolutely needs to be monitored by knowledgeable healthcare professionals, because real weight loss is not benign. Type 2 diabetics, for example, who lose weight by compliance with a total food replacement diet programme, will induce remission of their diabetes within a few days and continuing with hypoglycaemic medication can result in hypoglycaemia.
There are multitudes of patients taking drugs with a very narrow safety spectrum, such as warfarin or lithium. Dieting can alter the absorption of these drugs, so dosages need to be carefully monitored. There are some people who really should not be dieting at all. Pregnant women, patients with a recent history of surgery, stroke or heart attack are not logical candidates for weight loss.
Weight maintenance requires attention and is not usually possible in a busy medical practice. Long-term support in a pharmacy increases the weight maintenance prognosis for dieters.
Now or never
According the the Royal Pharmaceutical Society, it is ‘Now or Never’. “Pharmacists need to become first and foremost providers of patient care, rather than dispensers and suppliers of medicines This is central to securing a future in which the profession can flourish,” it says.
To be a ‘Today’s Pharmacist’ and have your pharmacy remain a valued destination on the high street, start developing and promoting your one-on-one services now. For patients to recognise and value your services, use your consultation room for patient services and not storage space. Be properly equipped for a weight management service by having weighing scales comparable to the ones we provide, that can weigh patients up to 32 stone. Have a chair in the consulting room with no arms that is strong enough to support an obese patient. Be professional, knowledgable, understanding and effective with your weight service.
The pharmacists of tomorrow will have a much greater opportunity to make use of their extensive pharmacy education, long after the vending machines have dominated the prescription business.
PDF Version: todayspharmacist
Govtoday Kreitzman masterclass
OBESITY PREVENTION AND TREATMENT ON THE HIGH STREET
S. N. Kreitzman Ph.D, R.Nutr.
Howard Foundation Research
Treating overweight, but not-yet-obese people, in pharmacy, is obesity prevention on the high street. There are over 30 million overweight and obese people in the United Kingdom. Since no one ever became obese without first being overweight, it is important to provide real help to people at this stage. It is much less problematic to help people who do not have a massive amount of weight to lose and who also do not yet have some of the serious medical consequences associated with excess weight.
Pharmacy has become the prime location for weight management in the UK and Ireland. With the NHS ‘Call to Action’, pharmacy professional bodies are urging pharmacists to make their voices heard and shout about the good they do in improving people’s health. Take weight management for example. Helping people lose weight is not just about making them feel good but is also about preventing major long-term health problems, such as type 2 diabetes. This point was very well illustrated in a recent article in GP magazine that reported a staggering sevenfold rise in insulin use in type 2 diabetes over a nine year period.
But it seems that it’s not just the NHS that needs to hear what pharmacy has to say. The public do too. North London LPC was inundated with enquiries about a newsletter it had produced raising awareness of pharmacy services in the area.
So what does that mean to you as a pharmacist with a team already offering an established weight management service? Promote your service far and wide and show the public and the NHS what you’ve been doing to improve the health of the nation.
Fin McCaul, for example, is first and foremost a community pharmacist practicing in Manchester. He is also the Chairman of the Independent Pharmacy Federation and works for Bury CCG one day per week as its Long Term Conditions Lead.
Fin’s passion for independent pharmacy is second only to helping patients lose weight and stop smoking. With an average of 100 quits per year and well over 1000 patients helped through the weight loss service in his pharmacy, there is nobody better placed to talk about the opportunities and challenges for pharmacy now that Public Health commissioning has moved into the care of Local Authorities.
Delegation, motivation and marketing skills and advice for pharmacists and their team are just some of the benefits from his Stop Smoking/Weight loss clinics. At the 2013 Pharmacy show he organised a series of Patient Services Workshops delivered by Pharmacists who are successfully running weight services in their local community and want to share their knowledge and expertise.
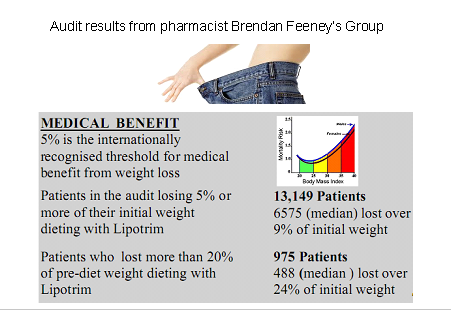
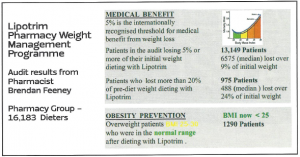
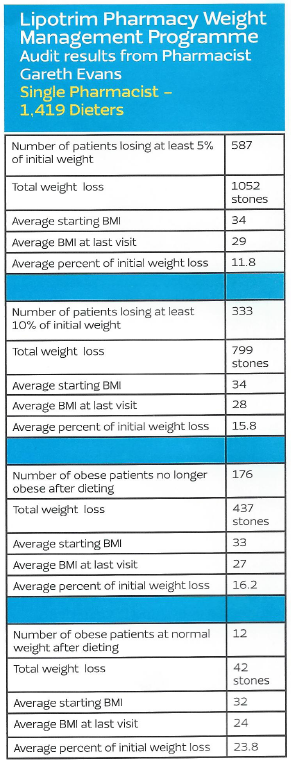
Fin’s expertise and results are not just anecdotes. He, along with many of the pharmacies treating overweight and obesity are generating extensive audit data from their weight management services. Results from one of his pharmacy audits below show the percentage of initial weight lost by over 1100 of his patients.
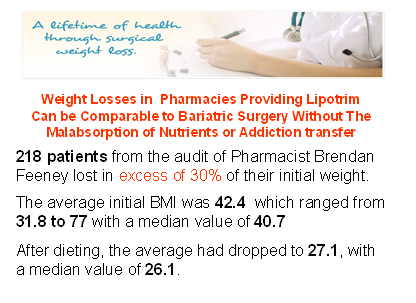
Pharmacy is an excellent provider of weight services for the community. Many overweight people in the BMI 25-30 range take advantage of pharmacy weight loss programmes recognising that they really work and confident that they are being monitored by healthcare professionals. Pharmacists’ expertise in weight management, however has proven extremely valuable for the treatment of obese and even the morbidly obese people. This is a group who could have qualified for bariatric surgery at great expense, risk and often compromised future life.
Effective weight loss absolutely needs to be monitored by knowledgeable healthcare professionals, because real weight loss is not benign. Type 2 diabetics, for example, who lose weight by compliance with a total food replacement diet programme, will induce remission of their diabetes within a few days and therefore continuing with hypoglycaemic medication can get them into serious difficulty. There are multitudes of patients taking medications such as warfarin or lithium, drugs which have a very narrow safety spectrum. Dieting can alter the absorption rate for these drugs so these patients need their dosages to be carefully monitored. There are some people who really should not be dieting at all. Pregnant women, patients with a recent history of surgery, stroke or heart attack are not logical candidates for weight loss. Effective weight loss should not be left to amateurs or internet sales. Healthcare professionals are needed, especially in pharmacy where continuous care can be provided even after the weight is lost, because weight maintenance requires the greatest attention and is not usually possible in a busy medical practice and appears to be almost impossible without professional help.
Although it is traditional to show successful dieters proudly occupying trousers which are now several sizes too large, there isn’t enough space to print over 13,000 examples. Results from this single audit of a group of pharmacies out of a collection of more than 2000 UK and Irish pharmacies currently treating overweight and obesity, is a vivid demonstration of the evidence base being accumulated for this absolutely essential community service from pharmacy.
Pharmacy is the only reliable community service providing and documenting long term weight management without the need major research grants or health service funding. Although there has been widespread press coverage for a £2.4 million grant by Diabetes UK to attempt to demonstrate that type 2 diabetes can be put into remission by effective weight loss, a fact that has been repeatedly reported in the medical press for over 30 years, pharmacies have been quietly and routinely succeeding with diabetes prevention and remission in their high street branches. Unlike bariatric surgeons, who need to justify the cost and risk of providing weight loss by surgical means on the basis of the phenomenal cost savings on the treatment of diabetes alone, weight loss in the pharmacy can accomplish the same results without massive expense and risk. And since total food replacement methods remove the substances of abuse for prolonged periods of time from those who may be suffering from a dopamine response to eating excess in their nucleus accombans , they don’t show the common addiction transfer syndrome that seems to be so common after bariatric surgery.
While activists continue to bellow about the size of soft drink containers, pharmacists are demonstrating how much their education and skills can be amplified by the convenience of access on the high streets of the UK. Pharmacy stands alone among the healthcare professionals in providing fantastic public health services such as smoking cessation, weight management, diabetes recognition, prevention and even treatment, medicines review, hypertension assessment and a host of other essential services very much needed in the real world. A major thank you is overdue.
PFD version: OBESITY-PREVENTION-AND-TREATMENT-ON-THE-HIGH-STREET
Getting great results from your weight management service- how I did it
Brendan Feeney, M.P.S.I, Community Pharmacist, Markievicz Pharmacy, Sligo
Valerie Beeson: Commissioning obesity support from the private sector
Counteracting Overweight, Diabetes and Hypertension in the Pharmacy
AN EFFECTIVE WEIGHT MANAGEMENT SERVICE IN PHARMACY
S. N. Kreitzman Ph.D. R.Nutr, V. Beeson, S.A Kreitzman Howard Foundation Research Ltd
Obesity is an issue that is now of critical concern to our increasingly overweight society. It is also an area where pharmacists have a real public health contribution to make. Being overweight or obese isn’t a mere cosmetic problem; it greatly raises the risk for other health problems, including High Blood Pressure, Coronary Heart Disease, Type 2 Diabetes. Stroke, Abnormal Blood Fats, Metabolic Syndrome, Cancer, Osteoarthritis, Sleep Apnea, Obesity Hypoventilation Syndrome, Reproductive Problems, Gallstones and more.
At a time when there is increasing competition for over-the-counter sales and decreasing revenue from prescriptions, weight loss offers an area where pharmacists are able to maximise use of their unique skills and training; offering their customers something that simply cannot be purchased from a supermarket or an online retailer. An effective weight loss service is perhaps the single most important contribution pharmacists can make to their community; certainly it is one of the most rewarding – both professionally and financially.
There are now more than 2000 pharmacies in the UK and Ireland offering the Lipotrim weight management service. The results they are achieving are not only comparable to that which can be achieved with bariatric surgery, they are also able to offer a supported programme for weight maintenance obesity prevention- something that is beyond the remit of surgery.
Of particular value is the contribution these pharmacies are making to the treatment of type 2 diabetes, Any patient taking oral mediations for diabetes must, in conjunction with their GP, stop the medication prior to dieting. The blood sugars often normalise within a few days and, with a stone or more weight loss, the diabetes is likely to remain in remission. Excess weight is a major promoter of type 2 diabetes and weight loss is well known to be an effective treatment.
Less dramatic, but equally important is the impact of weight loss on hypertension. It is estimated that in around 50% of cases with high blood pressure, the hypertension is weight related and responds favourably to weight loss.
With the Lipotrim service it is easy to document a pharmacy’s success. Audits can be completed virtually instantly, on demand, and with considerable flexibility. Secure audits can be completed within a single pharmacy or pharmacy group and even for the patients of a single surgery, providing evidence of the value of the service to local doctors.
The NHS is currently engaged in a losing battle against obesity, hypertension and diabetes in UK society. The runaway cost of treating these conditions is on the verge of bankrupting the health service, and still the numbers are trending inexorably in the wrong direction. Pharmacists are having a real impact on this battle by offering an effective alternative to NHS solutions to the problem (medication and bariatric surgery). Lipotrim is a cost-effective and highly successful weight management programme that is demonstrably providing fundamental health benefits for pharmacy customers, and profits for the pharmacies themselves.
PDF Version: infarm nov 2013