Tag Archives: VLCD
Very low calorie diets in diabetes: the Bournemouth experience
Pat Miles, David Kerr
Introduction
The therapy of obese patients with poorly controlled diabetes is a complex area. Despite the best efforts of healthcare professionals and patients, therapy is too often associated with repeated failure, which can give rise to frustration and sometimes despondency. Very low calorie diets (VLCDs) have been advocated for this population group. This article looks at the process and outcomes of one VLCD programme. The results support the wider adoption of VLCDs, but there are significant resource implications which are also discussed.
The treatment of the obese individual with poorly controlled diabetes is a common and perplexing problem. Wading in with ever increasing amounts of insulin without giving thought to ameliorating the inevitable weight gain will cause desperation in the multidisciplinary team and despondency in the patient. Very lowcalorie diets (VLCDs), of <800 kcal perday, are designed to achieve substantial weight loss while preserving lean body mass and are typically associated with a 20 kg weight reduction in three months (NTFPTO, 1993). Unfortunately, regain of half to two-thirds of the initial weight loss is common within 12 months after cessation of the diet, although there may be longer term benefits in terms of a reduction in the need for medication in obese individuals with diabetes (Wing et al, 1994). Recently, Paisey et al (1998) compared VLCD with a traditional intensive dietary regimen in 30 obese (BMI>30) patients with diabetes and 19 obese controls without diabetes. After four months of VLCD, subjects were switched to a low-fat diet and continued to be seen weekly by the multidisciplinary team. Weight loss was substantial and maintained after cessation of VLCD (mean 14kg at 12 months), and 14 of the 15 patients who had chosen VLCD had normal blood glucose and fructosamine levels despite stopping all medication. For four patients with recent-onset diabetes, normalisation of blood glucose levels was sustained for 12 months.
Study aim
A pilot study was carried out to examine the effect of a VLCD programme on a group of obese (BMI30) patients with diabetes. These patients remained obese despite enormous efforts by the multidisciplinary team (including primary care). Usually, there was also poor glycaemic control. Method Between January and June 1999, 24 patients aged 29–76 years were enrolled into Lipotrim (Howard Foundation Research, Cambridge, England), a VLCD programme which gives 450 kcal per day for women and 600 kcal per day for men. For entry to the programme, each patient had to:
- Understand the programme
- Desire to take partUndertake to attend weekly individual and group sessions
- Have family support
- Be desperate or determined to lose weight.
The product was available from the hospital at a cost of £18 per week for women and £24 per week for men. The expenditure for each patient was offset against money saved by not purchasing normal food. Lipid-lowering medication was stopped on entry to the programme. Weight, blood pressure and urinary ketones were measured once weekly up to refeeding then weight and blood pressure were measured at every patient contact thereafter. Lipid levels and HbA1c were measured at the start of the programme, every month for the first six
months then at three-monthly intervals for the next six months. Patients were expected to attend the individual and group sessions at each visit (every week). In the individual sessions with the nurse, patients could discuss any problems they had encountered (Figure 1). Group sessions provided support, an opportunity to exchange experiences and preparation
for refeeding. The dietitian was involved around the time of refeeding, to reinforce product literature from the company. Most patients refed at 3–4 months, and then followed a low fat healthy eating plan. After refeeding, follow up continued weekly for the first month, then every 2–4 weeks (frequency at the patient’s discretion). However, group sessions stopped at six months into the programme.
Results
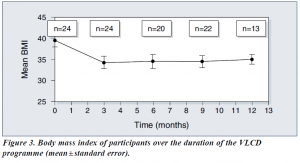
Average body mass index (BMI) was 39.5 at the start of the study.
Of the 24 patients:
- 16 were being treated with insulin
- 14 were hypertensive and were receiving appropriate medication
- 14 had dyslipidaemia and were receiving appropriate medication
- 2 were suffering from sleep apnoea requiring continuous positive airways pressure
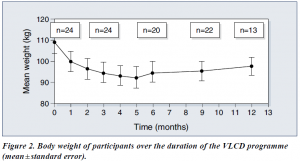
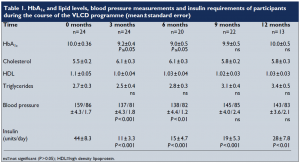
Following the introduction of VLCD, there were significant reductions in body weight (Figure 2) and BMI (Figure 3). Data on HbA1c levels, plasma lipids, blood pressure and insulin requirements of programme participants are shown in Table 1. Plasma lipid levels remained largely unchanged. Only four patients restarted lipid-lowering medication after refeeding.
Blood pressures dropped significantly within the first week, and adjustment of antihypertensive medication was necessary on a regular basis. Eleven patients stopped all antihypertensive medication. For most patients, ketone levels were moderate to high during the VLCD (indicating adherence to the programme and utilisation of fat stores). Insulin doses were decreased by two thirds on commencement of the programme, and this seemed to work well, with insulin doses continuing to decrease as weight loss proceeded. Most patients who remained on insulin were changed to nocte insulin
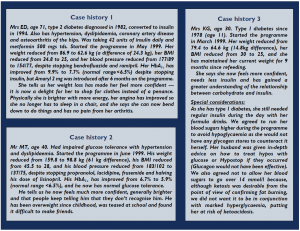
when their requirements were less than 14 units a day. Sulphonylureas were also halved or stopped on commencement of the programme. Only 13 patients completed follow up for the 12 months of the programme. The three case histories (see page 111) provide further detail about some of the patients in the programme.
Discussion
Benefits of VLCD
VLCDs can be an effective method of reducing weight, improving glycaemic control
— at least in the short term — and reducing the need for concomitant medication in
obese people with diabetes. They can also allow individuals to gain insights into the potential benefit of weight reduction and to learn about the relationship between food and obesity. When asked why this diet had worked while all others had failed, our patients said that it was easier to have no food at all, than to try to make choices from food offered, particularly on social occasions. Also the rapid weight loss experienced on the programme was positive reinforcement, together with the feeling of ‘wellbeing’ experienced as a consequence of ketosis (Burley et al, 1992).
Some considerations
It is well known, however, that helping someone to maintain weight loss is often the most difficult and disappointing task (Wing, 1995). In addition, the process is very time consuming for any healthcare professional involved. This pilot project to examine the effectiveness of VLCDs involved seeing 24 patients every week for 3–4 months, then at least monthly for the following nine months. We have only touched the ‘tip of the iceberg’ in our clinic population. If this service were offered to all of our obese patients (at least 60% of the total), a 50% uptake would involve 2250 patients who would require 11 whole time equivalent healthcare professionals just to provide weekly visits! In practice, this would be unrealistic and unlikely to attract funding, though one could argue that treating the root cause of the problem is far better than attempting to treat the effects. Putting VLCD into practice In many areas, primary care is offering Lipotrim to its obese patients. If the expertise of practice nurses and community dietitians in using this product could be built up, and the diabetes team was available for advice on medication changes for people with
diabetes, then it could be possible to offer this service more widely and cost effectively.
However, because of the additional risks of hypoglycaemia and ketoacidosis in patients with type 1 diabetes, we feel that they should only be offered the programme under the supervision of an experienced diabetes team, and then only if the patient is able to self-adjust insulin appropriately and understands the risks.
Conclusion
This study advocates the use of VLCDs for reducing weight and improving glycaemic control in obese people with type 2 diabetes (as well as carefully selected people with type 1 diabetes under close supervision). VLCDs can also reduce the need for concomitant medication. While on a VLCD, individuals can become empowered through their increased awareness and knowledge of their diabetes and the positive feedback provided by the rapid weight loss. It is likely that lack of time would limit the widespread adoption of the VLCD service used in this pilot study. However, the potential benefits of VLCD make it worthwhile to try to produce a costeffective service, perhaps by increased primary care involvement.
PDF Version: bournmouth-miles-kerr
Treating obesity is easy – just eat less (so the saying goes)
Positioning pharmacy as an effective option to bariatric surgery
Nov 2012
Recent NHS figures show that the number of people undergoing bariatric surgery has quadrupled in the last 5 years – from 1,573
people in 2006-07 to 6,723 in 2011-12.
Although bariatric surgery is very effective at producing rapid weight loss that causes type 2 diabetes to go into remission, it comes with a multitude of problems including high morbidity and mortality risk, prohibitive initial and followup costs and limited availability. However, there is a readily available alternative to bariatric surgery that is evidence-based, safer, much
more cost-effective and one where pharmacies are playing an active part: Very Low Calorie Diets (VLCDs) properly monitored by healthcare professionals.
The rise in bariatric surgery has led to prominent pharmacy figures Mike Holden, chief executive of NPA, and Ajit Malhi, AAH
Pharmaceuticals’ head of marketing services, arguing the case for pharmacy which is playing an increasingly prominent role in tackling obesity in the community, as part of the public health and Healthy Living Pharmacy drive.
With over 2000 pharmacies offering the Lipotrim VLCD programme, overweight people have ready access to a pharmacist who can not only help them reduce weight, but also assist them adopt healthier lifestyles, change eating and exercise habits and pre-empt or control existing diabetes.
Pharmacists therefore deserve considerable recognition for providing a service capable of promoting remission of type 2 diabetes and relief of co-morbidities, where present, without depleting the assets of the NHS. And, crucially, praise for the effective reatment of excess weight in hundreds of thousands of patients, where documentation of weight loss represents evidence for the value of pharmacy.
PDF version: ICP LIPOTRIM COLUMN Nov_ r2
Support GPs in tackling obesity
Feb 2013
The Royal College of Physicians (RCP) suggested in a report last month (Action on obesity: comprehensive care for all) that GPs
should direct obese patients to community services, including pharmacies, rather than offering in-house clinics. The report pushes for multi-disciplinary teams with pharmacists working alongside GPs, dieticians, counsellors and physiotherapists, and called for a national model for the commissioning of community services for obese patients.
This is further testament that pharmacists must be doing something right here.
Pharmacies have been running dedicated weight management services for over a decade. In the last couple of years the Royal
Society for Public Health has become more involved in pharmacy, and the NHS has given the nod to the Healthy Living Pharmacy initiative.
The big sticking point for pharmacy has been demonstrating value. But this has all started to change over the last couple of years with the introduction of the Lipotrim Patient Tracker, an online IT programme that keeps patient records for their weight management service and provides for comprehensive audits to be produced.
The evidence produced so far from Lipotrim pharmacies clearly shows that pharmacy offers a very successful and costeffective
service that will make a big impact in reducing the obesity epidemic and the costs to the NHS.
With only two months until clinical commissioning groups (CCG) take over from PCTs, it’s crucial that pharmacists embrace
and push for the RCP model to work and shout out about the evidence.
PDF Version: ICP LIPOTRIM COLUMN Feb_ r1
Offering pharmacy support behind VLCDs
Oct 2012
Not all Very Low Calorie Diets (VLCDs) are the same, and not all VLCD programmes are the same. Customers need to be made aware that some online VLCDs come without the proper formulations or essential support of a healthcare professional.
VLCDs should use nutritionally complete food formulas designed to replace all regular meals with no additions. The professional weight management programmes are especially valuable for the obese where the excess weight has led to co-morbidities such as type 2 diabetes, hypertension and mobility problems. They are not for the casual dieter who wants to shed a few pounds before going on holiday, but can help prevent overweight from progressing to obesity.
but weight loss can have an impact on existing medical conditions. Real weight loss should be managed in a healthcare setting where knowledgeable screening and weekly monitoring are routine.
Lipotrim is a professional VLCD programme that is only available from pharmacies and GP surgeries. The initial consultation involves screening for suitability and taking a careful medical and drug history. In some cases GP involvement is required, e.g. for stopping drugs in patients with type 2 diabetes. Patients are required to return to the pharmacy weekly for monitoring, counselling if necessary and to collect the next week’s supplies. People nearing their target weight are given lifestyle advice on
maintaining their weight and offered the followon maintenance programme.
Online VLCDs cannot replace the comprehensive care, support and expertise provided by a pharmacy‘s professional weight
management service. And importantly, online purchases cannot guarantee the compositional integrity of products that have at times been known to violate international standards for total food replacement products and programmes. Caveat emptor!
PDF Version: ICP LIPOTRIM COLUMN oct_
Capitalising on the post-Olympics healthy living drive
Sep 2012
The Government has been very keen on using the Olympics and Paralympics as a driver for getting more people doing sport and exercise and it seems that, with the post-games euphoria, people are taking up the opportunity of becoming more active.
But there is another driver to this health agenda – the cost to the NHS of the consequences of an unhealthy lifestyle, in particular diabetes. According to the latest figures from the Health and Social Care Information Centre (HSCIC), diabetes prescription numbers topped 40 million for the first time last year, a rise of nearly 50% in six years. That now puts the drugs bill for diabetes
at a staggering £760.3 million.
Health Minister Simon Burns responded to the report saying: “The number of people with diabetes has been rising for years, mainly because of an increase in the number of people who are obese due to a lack of exercise and unhealthy diets… it is so important that we take urgent action to tackle the problems caused by obesity.’’
Tackling obesity is something that pharmacy is proving to be well placed to do. It reaches further out into the community to get
the message across about healthy living, for example linking with local diabetic nurses or capitalising on current sports initiatives. And Lipotrim, with the unique Patient Tracker, now has documentation that, in parallel with bariatric surgery, the rapid weight loss induced with Lipotrim can often put type 2 diabetes into remission.
Lipotrim allows pharmacists to offer and document a very effective weight management programme that provides the eassurance of a healthcare professional selecting and monitoring patients, some of whom may have diabetes. And with the current Government push, now is a time for pharmacy to make a real difference.
PDF Version: ICP LIPOTRIM COLUMN sept_
Capitalise on HLP to drive your weight management service
May 2012
The Healthy Living Pharmacy initiative has far exceeded expectations, now having nearly 200 accredited HLPs in 20 pathfinder sites across 30 PCTs, with many more vying to get involved. In the meantime, the government’s Pharmacy and Public Health Forum chair Professor Richard Parish has told community pharmacy that ‘its time has come’ and urged it to capitalise on the opportunities out there.
Pharmacy has not had a bigger opportunity than this to make its mark in public health. HLP aims to improve the health and wellbeing of the local community through high quality pharmacy-delivered public health services, including weight management. The pathfinder sites’ remit will also be to build the evidence-base for pharmacy’s contribution to public health
before roll-out.
Lipotrim has been behind pharmacy’s public health role all along, developing its weight management service package to enhance pharmacy’s developing professional roles. And since introducing the service from the GP arena to pharmacy over 10 years
ago, Lipotrim now has more than 2000 pharmacies offering the service, this represents a strong body of evidence to support pharmacy’s role in weight loss.
Foreseeing the value of evidence, the company has also developed the Lipotrim Pharmacy Patient Tracker to make it easy for each pharmacy to audit its own service and demonstrate value. For anyone looking to get involved in HLPs and use it to drive
their weight management service, this will be an invaluable tool.
PDF Version: ICP LIPOTRIM COLUMN May r1
Promoting weight management alongside your stop smoking service
Mar 2012
All the publicity surrounding No Smoking Day (March 14th) gives you a great opportunity to advise on healthy eating and promote your weight management service.
Smokers considering quitting are often deterred by the potential of weight gain.
Not all quitters gain weight and the exact mechanism is poorly understood, but has been linked to the fact that nicotine may suppress appetite and increase metabolism by a small amount. Food can also be used as a comfort by quitters and as a replacement to the habit and addiction of smoking. For people that are concerned, the advice should be about the overwhelming benefits of quitting, the need to eat healthily and how they can manage their weight if this becomes a problem.
The pharmacy is in a unique position in being able to offer support on these two inter-linked pharmacy services. The pharmacy
team should be on the lookout for customers who decide not to stick with the stop smoking programme because of worry about weight gain. Normal weight people will be assured of remaining weight stable after quitting using the Lipotrim maintenance formulas and healthy eating. Likewise people who are trying to lose weight and give up smoking at the same time may need more in-depth counseling and the strict weight loss service.
The Lipotrim Pharmacy Programme offers a range of diet products and maintenance products to support these customers. The
Patient Tracker can also be used to show weight loss or stability over time and encourage them to remain quitters.
PDF Version: ICP LIPOTRIM COLUMN march r1
Setting up a successful weight management service
Feb 2012
A weight management service can help you meet both your professional and business objectives. The first step to setting up your service is to recognize the business opportunity as well as the professional contribution you can make to the health of your community. Pharmacy is a primary healthcare provider for weight management services and the widespread need for effective weight control will direct customers to the pharmacy providing the most effective service. Properly run, a weight management programme will substantially increase footfall and lead to extended customer loyalty. Decide on a service specification that will provide the evidence of efficacy, the equipment you need and the SOPs, staff training and continued support for your programme.
You need to think about how you bring the customers in. In-store posters and leaflets, local GP surgeries and sports centres and tie-ins with national campaigns are all good sources of new business, but the best source of new people is the impact successful dieters have on their relatives, friends and acquaintances. Paying proper attention to the protocols of the programme will pay off big time.
And don’t forget about evaluating your service and the positive health outcomes to your population. Gathering evidence for this puts you in a strong position for further funding from local commissioning groups and getting involved in the Healthy Living Pharmacy initiative.
Lipotrim Pharmacy supports you in all the above, from training and CPD, to tools to promote your service and right through
to evidence gathering thanks to the Lipotrim Patient Tracker.
PDF Version: ICP LIPOTRIM COLUMN feb r1