Stephen Kreitzman Ph.D, R.Nut. (UK Registered Nutritionist) & Valerie Beeson
Howard Foundation Research Ltd. Cambridge UK
It should be reasonable to justify practice time and resources to assist overweight and obese patients lose their weight. The link to type II diabetes alone is sufficient. With rapid weight loss, normalisation of blood sugar
levels is achieved in days and with further weight loss, the disease can be held in remission. Better long term glycaemic control is achieved with rapid weight loss, even after some weight regain, than is achieved with the same weight lost more slowly. About 50% of hypertensive patients can reduce drug treatments with weight
loss. Surgical interventions can be scheduled when substantial weight is lost. Fewer anti-depressants are required and overall, the frequency of GP visits is significantly lower for leaner patients.
There is no shortage of choice to meet the weight loss needs of individual patients. Drugs, both current and promised for the future, dietetic referral, exercise on prescription, and pharmacy based treatment programmes are all needed in order to deal with the massive problem of obesity. Each has a place depending upon the specific clinical needs of the patient. An exercise prescription may not be the best choice for a 40 stone patient who may struggle simply to walk, which at this weight is considerable exercise. Weight loss has been advocated as an adjunct to treatment for patients with conditions such as diabetes type 2, hypertension,
osteoarthritis and a catalogue of other disabilities. Generally, little attention is paid to this option because of the difficulty patients have experienced in losing adequate amounts of weight and keep it off. The widespread availability of effective weight loss programmes in UK and Irish pharmacies, however, argues strongly for offering overweight patients, especially type 2 diabetics, an opportunity to try a course that leads to less dependence on drugs and frequently leads to long term remission of disease.
Diabetes type ll is nearly 100% reversibly related to excess weight
For diabetes, there are really two basic facts to consider. The first is that type II diabetes is a disease that has a primary etiology which is close to 100% REVERSIBLY related to excess body weight. The second fact is that diabetic patients can lose enough weight within a few days to bring their blood sugars under control and enough further weight within weeks to crucially reduce cardiovascular risk factors and apparently keep the disease in remission, even with some weight regain.
WEIGHT SPIRAL:
Standard treatment for type 2 diabetes, with emphasis on using drugs to lower the blood sugar levels, often results in a relentless vicious circle. High blood sugar leads to drug intervention, which results in increased body weight, which in turn elevates the blood sugar, which increases the requirement for more potent drugs,
which spirals to obesity and possible insulin dependency. Patients are getting fatter as a result of treatment and this necessitates more aggressive rug usage. With significant weight loss, drug usage can be reduced and in many cases stopped permanently.
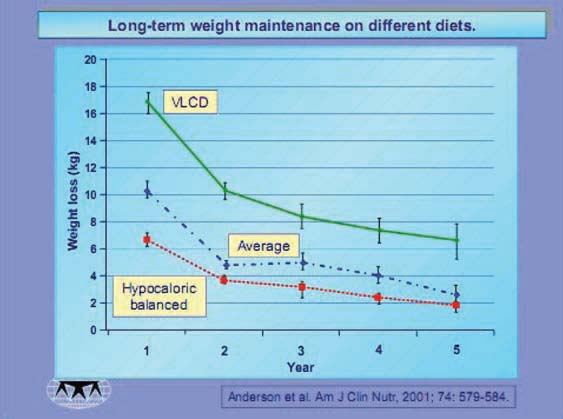
LONG TERM WEIGHT MANAGEMENT
While willpower can often help people lose weight over a short defined period, control for the months, years or even decades required for stability is quite a different story. Loss of weight by any means confers absolutely no
lasting legacy for weight maintenance. Weight loss, however achieved, is only the beginning of the treatment, not the end point. When the drug therapy is discontinued. When the counsellor moves on. When the patient is “cured” of excess weight. This is the point at which a dieter requires the maximum attention and assistance.
Weight management requires control of eating behaviour over a sustained period of time and the implementation of lifestyle changes. Justifying practice time and resources for a patient who has achieved weight loss and is now both healthier and at a normal weight is difficult. The expectation that this patient will sustain the weight loss without considerable help, however, is naïve. Pharmacy based programmes are ideal for the varying long term weight management needs of patients.
Obesity prevention can also be part of the pharmacy contribution to health promotion services; dealing with excess weight before it reaches obese levels and exacerbates comorbidities. The care of patients during
weight loss, is advantageous when monitored by a pharmacist, who understands the implications of other drug
treatments that may interact with the weight loss programme. But it is at the post diet stage that the pharmacist
is best equipped to provide essential long range guidance, support and education that will increase the
length of time that the weight loss is maintained.
Both the new GP and the pharmacy contracts strongly encourage interactive efforts to deal with a range of health problems, most of which have weight related implications. Weight loss is vital for management of, cholesterol, blood lipids, diabetes, hypertension or asthma. It even impacts programmes for smoking cessation.
ACHIEVING A MAXIMUM SAFE RATE OF WEIGHT LOSS
Modest reductions in Calories can theoretically result in weight loss. Of course, the modest reduction has to be from the equilibrium level, not from current intake. If a person is overeating by 2000 Calories a day (very common in the obese), a modest reduction in Calorie intake will not cause weight loss.
There is a maximum rate of weight loss for any individual. A total fast provides zero calories and therefore requires that all the Calories necessary for life come from the body fuel reserves. A total fast, however, provides no nutrients and since an obese patient has a far greater reserve of calories than stores of other essential nutrients, a total fast is out of the question as a treatment. To be healthy, a diet has to supply
adequate essential amino acids, essential fatty acids, vitamins, minerals and trace elements. A total fast cannot be a valid treatment for obesity. The simple idea of reducing fat levels in an enteral formula solves both the Calorie and the nutrient problem. An ideal nutritional product with the absolute minimum of Calories consistent with a healthy diet is achieved. Lipotrim is an example of such a product, providing a maximum safe rate of weight loss. The literature on safety and efficacy is massive. The time has really come to pay attention to it.
BENEFITS OF WEIGHT LOSS
There is also an extensive literature on the beneficial effects of weight loss on cardiovascular risk factors, on blood lipid profiles and blood pressure. Managing weight in general practice is time consuming. The beneficial results from reliable weight loss on the glycaemic control and the cardiovascular risk factors more than justifies pharmacy cooperation. It benefits patients and makes good use of pharmacists’ training and facilities.
Weight is extremely important to patients generally and has a critical influence on the clinical course of many medical conditions. Uniquely, however, with type II diabetes, because the blood sugar can normalize so quickly under conditions of rapid weight loss, it is essential that hypoglycaemic medications are stopped prior to dieting. This requires an understanding, on the part of the prescribing GP, of the need to stop drug treatment and follow up of the patients.
THE IMPORTANCE OF PHARMACY IN WEIGHT MANAGEMENT
The need to deal with excess weight is no longer simply a cosmetic issue. Obesity has become pandemic. The serious consequences of excess weight are being acknowledged as type 2 diabetes rates soar in children as well as adults. There is probably no other service that a pharmacist can provide that will prove to be as valuable to the needs of general practice as weight management. When effective self-funding programmes are available that do not require allocation of scarce resources from PCTs, it is hard to imagine any pharmacy failing to cooperate with a weight management programme. The problem has become so pervasive, that it will take a wide variety of treatments, drugs and public education to have any impact. Hospital programmes for weight management are overwhelmed. Pharmacy is the best community resource and pharmacists’ training ideal for providing professional assistance in dealing with the major health issue of the decade.
REFERENCES
Wing RR, Blair E et al. Calorie restriction per se is a significant factor in improvement in glycemic control and insulin sensitivity during weight loss in obese NIDDM patients. Diabetes Care 17:30-36,1994.
Wing RR, Marcus M & Bononi P. Glycemic control after weight loss is affected by how weight loss is achieved. Diabetes, 39: suppl 1, 50A,1990.
Wing RR, Marcus MD, Salata R, Epstein LH, Miaskiewicz S & Blair EH. Effects of a very low calorie diet on long term glycemic control in obese type II diabetic subjects. Arch Int Med, 151: 1334-1340, 1991.
Weck M, Hanefeld M & Schollberg K. Effects of VLCD in obese NIDDM (noninsulin dependent diabetes) on glucose, insulin and C peptide dynamics. Internat J Obes, 13: suppl 2, 159-160, 1989.
Uusitupa M, Alaakso M et al. Effects of a very-low-calorie-diet on metabolic control and cardiovascular risk factors in the treatment of obese non-insulindependent diabetes. Amer J Clin Nutr. 51:768-773,1990.
Shaper AG, Wannamethee SG & Walker M. Body weight: implications for the prevention of coronary heart disease, stroke and diabetes mellitus in a cohort study of middle aged men. Brit Med J, 314: 1311-1317, 1997.
Reports on tasks for scientific cooperation (EU SCOOP)
Report of experts participating in Task 7.3, September 2002 Collection of data on products intended for use in very-low-caloriediets Directorate-General Health and Consumer Protectionz
PDF version: 2-4-obesity-pandemic