DIABETES ACHIEVING WEIGHT MAINTENANCE
AFTER SUBSTANTIAL VLCD WEIGHT LOSS
S.N Kreitzman Ph.D, R.Nutr. (UK Registered Nutritionist),V. Beeson & S.A Kreitzman Howard Foundation Research Ltd. Cambridge UK
WEIGHT MAINTENANCE AFTER WEIGHT loss is perfectly possible, but not often achieved by traditional hypoenergetic diet programmes. Considering the paucity of evidence to support the idea that there is maintenance benefit from a slow rate of weight loss and the considerable amount of contrary evidence, it is very surprising that this idea persists.There is now recognition that even bariatric surgery suffers from unexpectedly high rates of recidivism after initial weight losses; this should have already altered the widespread expectation that weight maintenance should necessarily follow successful weight loss.We have reached a stage where VLCD and bariatric surgery are available to produce sufficient weight losses to promote medical benefits.At the top of the extensive list of co-morbidities associated with excess weight is type 2 diabetes. In order for these medical benefits to be sustained as long as possible, rapid weight loss and a structured, effective, maintenance programme are vitally important.
Weight regain after dieting can result from a variety of causes.The simplest of these is also the most common.The physiological principle here is that early weight losses are almost entirely due to the utilization of sugar and glycogen.These carbohydrate fuels with their associated bound water are regained quickly after restoration of normal eating, There is only a minimal actual change in fat storage — only small amounts of fat weight are lost, even when there may be a reasonable amount of weight loss due to depletion of the stored glycogen and its associated water. Lack of attention to an appropriate, structured, re- feeding can lead to carbo-loading, in a manner similar to the effect sought by endurance athletes.The consequence to a dieter; however is an excessive repletion of glycogen with its substantial rebound hydration.This can often produce weight regain in excess of the weight lost, and is a common feature after intermit-tent calorie restriction.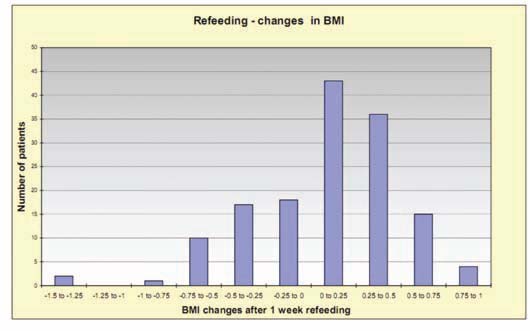
With a correct refeeding strategy, weight maintenance is much more assured.’Carbo loading’ requires depletion of glycogen followed by intake of high glycaemic index carbohydrate foods. Athletes often consume pasta, but fruit, bread, cereals etc. are just as effective.The result is a rapid overload of stored glycogen, often more than twice the pre-depletion levels.When the additional glycogen becomes bound to water for storage, considerable weight gain can be achieved.This is not a problem for an endurance athlete who will soon utilize the extra glycogen, but a considerable blow to a dieter who has just sustained prolonged food restriction in an attempt to lose weight.
Evidence for weight stability during a week of properly structured refeeding is demonstrated from an audit of patients attending a pharmacy based programme.
| Before | After | |
| Refeeding | Refeeding | |
| Valid cases | 146 | 146 |
| Mean BMI | 27.45 | 27.39 |
| Median BMI | 26.63 | 26.57 |
While there are indeed some minor variations in individual stability of BMI following the re-introduction of normal foods and re-establishing normal glycogen stores, these differences are usually trivial.
“New NHS research has revealed the shocking toll of preventable deaths caused by just one medical condition — diabetes — which is causing 24,000 needless deaths a year in England alone. It’s not just the old and middle-aged who are at riskYoung women with diabetes are 6 to 9 times more likely to die than their age group overall. And many more young people who don’t die will develop life threatening diseases later due to failure to manage their blood sugar. Badly controlled diabetes can lead to kidney disease, heart conditions, or blindness. It’s also the cause of 5,000 amputations a year mainly of legs or feet.With around 3 million diagnosed sufferers known to the health service, diabetes is said to be costing the NHS £9 billion a year about a tenth of the total health budget.”
File on Four. BBC Radio 4, 21 February 2012
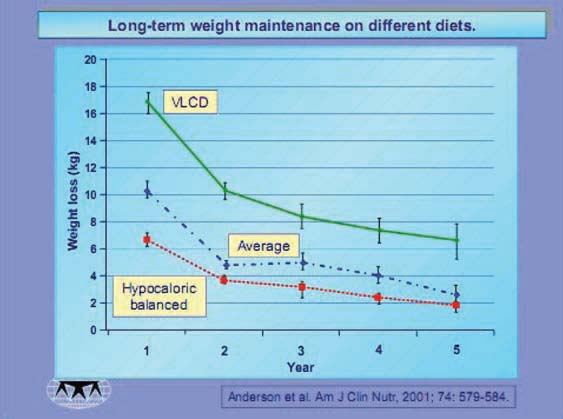
Fig. I Design:Studies were required to I) have been conducted in the United States, 2) have included participants in a structured weight-loss program, 3) have provided follow-up data with variables estimates for y. Primary outcome variables were weight-loss maintenance in kilograms, weight-loss maintenance as a percentage of initial weight loss, and weight loss as percentage of initial body weight (reduced weight).
Weight Maintenance after Dieting
Weight loss with VLCD is especially beneficial for minimizing recidivism after substantial weight loss
Weight recidivism, when substantial weight loss has been achieved, can represent a more fundamental physiological problem. It is becoming increasingly accepted that food can become a substance of abuse, and that it shares the pathways common to addictions associated with tobacco, alcohol and drugs. It is an extremely rare occurrence when addicts are able to slowly wean themselves from the abused substance. Stopping the substance of abuse is the most effective strategy for almost all addictions, but there are serious consequences associated with a total cessation of food intake. In cases where the weight problem has become substantial enough that addictive mechanisms are likely, a case may be made that very low calorie formula diets (VLCD) are the only weight loss method with any real chance of succeeding, especially into the critical post-diet period.With a nutrient complete formula replacing all traditional foods, there is interference with the addictive processes and the dieter has a greatly improved chance for successful weight maintenance. Evidence that VLCD confers bet-ter long term weight maintenance than traditional hypoenergetic balanced diets has been repeatedly published.A particularly careful assessment was published in the American Journal of Clinical Nutrition in 2001 by James Anderson and co-workers.The report “Long-term weight-loss maintenance:a meta- analysis of US studies” compared 5 year post diet maintenance from published structured weight loss programmes. As can be seen from figure I . above, from 29 published studies that met the inclusion criteria, there was considerably more weight lost by the VLCD

Fig. 2 Many pharmacies in the UK using the Lipotrim PatientTracker software also track weight maintenance after completion of the weight loss programme. Results from Pharmacist Gareth Evans, for example, emphasize that post diet changes in BMI are minimal for the vast majority of dieters.
studies. After 5 years, the VLCD subjects still sustained a greater weight loss than the initial loss from the hypocaloric balanced diet.The criteria are described in the study design.
Maintenance of the weight lost is particularly important when treating a patient with type 2 diabetes.With the combination of rapid weight loss and a reliable maintenance opportunity,
VLCD are a vitally important option for the management of diabetes.
GPs already know the extent of the problem. Diabetes in particular, fuelled by an epidemic of overweight and obesity, is undermining the nation’s health. But it has been shown that with the aid of a very low calorie formula diet (VLCD), rapid weight loss leads to rapid remission of type 2 diabetes. A one-year study showed that BMI of obese diabetic patients was reduced by 5kg/m2 and that patients were able to discontinue insulin and oral hypoglycaemic agents for the whole year.2 A five-year follow-up study confirmed that VLCD treatment was safe and effective in overweight diabetic subjects. It has also been shown that normalisation of both beta cell function and hepatic insulin sensitivity in type 2 diabetes is achieved byVLCD dietary energy restriction.
PDF Version: 2-2-napc_2012-maintenance